Neonatology
Session: Neonatal Quality Improvement 6
87 - A Quality improvement bundle to improve outcomes in periviable infants at a level 3 community neonatal intensive care unit
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 87
Publication Number: 87.2836
Publication Number: 87.2836

Abhinav Pal, MD`
Neonatologist
Stormont Vail Hospital
LAWRENCE, Kansas, United States
Presenting Author(s)
Background: Rates of survival for infants born at the border of viability are still low and vary considerably nationally
Objective: Our primary objective with this quality improvement initiative was to improve survival to hospital discharge rates and outcomes for infants born at 22 -24 6/7 weeks gestation.
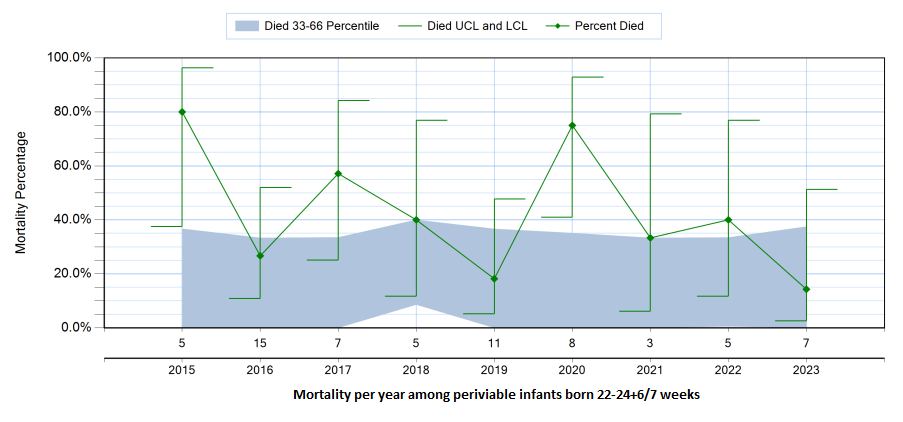
Design/Methods: The quality improvement initiative was conducted from January 2021 to September 2023 at Stormont Vail Hospital neonatal intensive care unit (NICU). All actively treated infants born from 22 + 0/7 to 24 + 6/7 weeks' gestation were included. The primary outcome was death or severe Intraventricular hemorrhage (IVH) in the primary population. For comparison, baseline data from 51 infants born at 22-24+6/7 weeks was obtained from 2015-2020. QI bundle consisted of education, simulation, availability of equipment and changes in protocol. Physician and nursing education consisted of establishing protocols for early antenatal steroids at 21 weeks gestation, standardized ventilator management, management of patent ductus arteriosus and golden hour. Outcome and process measure data were analyzed by using p-charts.
Results: 15 infants with gestational age 22 - 24+6/7 weeks gestation were born between 2021-2023 during the study period. Birthweight ranged from 376g-800g. All infants received at least one dose of antenatal steroid. Overall unit mortality for periviable infants decreased consistently over years from baseline of 43% to 27% in 2021-2023 (survival increased by 16%; p=0.01). Severe IVH decreased from 27% to 20%. Rate of chronic lung disease remained similar (23% vs 20%, p=0.2). Rate of Necrotizing enterocolitis (NEC) seen in our cohort was high at 13% compared to baseline of 2%. Late onset sepsis remained similar at 13% compared to prior years.
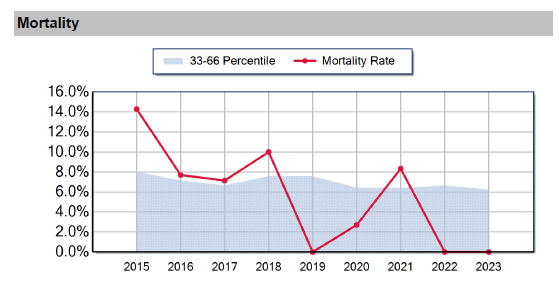
We also saw improved outcomes in infants born at 25-28 week population during the study period. In this group, there was decrease in mortality from 7% to 4%(p=0.03) and the rate of severe IVH decreased from 9% to 6%.
Conclusion(s): Implementation of a bundle of evidence-based practices, availability of smaller equipment and consistent care was associated with decrease in mortality and severe IVH. As an added advantage, improved care of periviable infants also led to improved outcomes in older gestational age infants
.png)
