General Pediatrics
Session: General Pediatrics 2
251 - The Great Disconnect: Examining Adolescent-Provider Communication Preferences in Mental Health Care
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 251
Publication Number: 251.542
Publication Number: 251.542
- JB
Joshua Broadman, MD (he/him/his)
Pediatric Resident Physician
University of Florida College of Medicine
Jacksonville, Florida, United States
Presenting Author(s)
Background: The surge in mental health (MH) issues among adolescents emphasized the critical need for accessible care. The evolution of telehealth transformed healthcare delivery, though some teens remain hesitant to engage openly with physicians in face-to-face (F2F) encounters. Further research is required to understand adolescent barriers to disclosing MH issues, thereby enabling improved healthcare.
Objective: We conducted a mixed-methods study to investigate physician and adolescent preferences and perceptions regarding the discussion of sensitive information. The research aimed to uncover barriers to MH disclosure and assess trust and comfort in the doctor patient relationship. Additionally, we explored perceptions of a novel communication method to facilitate clinical MH conversations.
Design/Methods: We recruited physicians (n=101) and adolescents (n=100) to complete targeted questionnaires. Physicians were recruited online and with flyers, adolescents at local clinics. Survey questions were derived from peer reviewed studies on doctor-patient communication. We employed descriptive statistics to summarize participant characteristics and perceptions. We performed thematic analysis using NVivo10 to identify recurring themes/patterns.
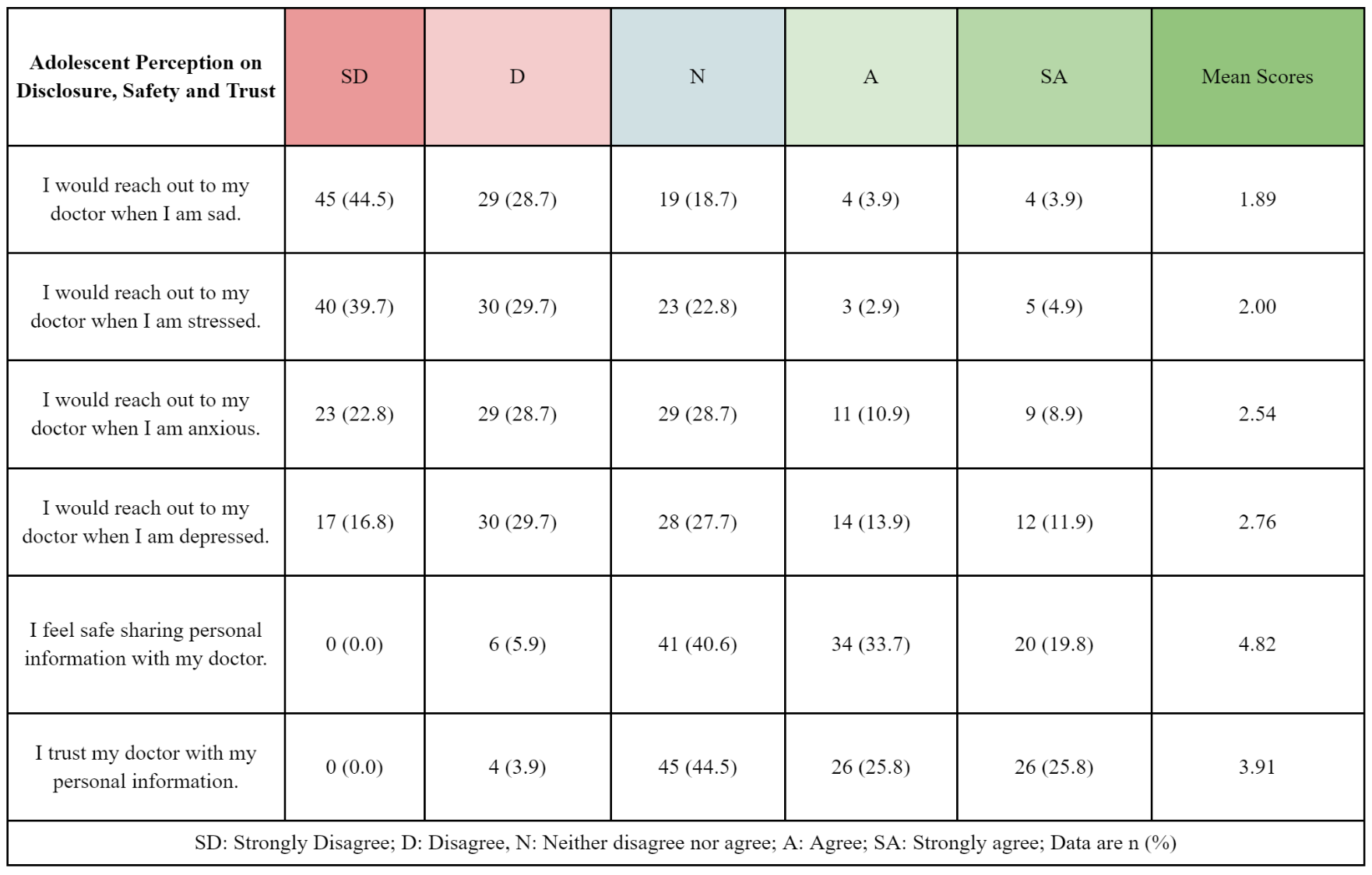
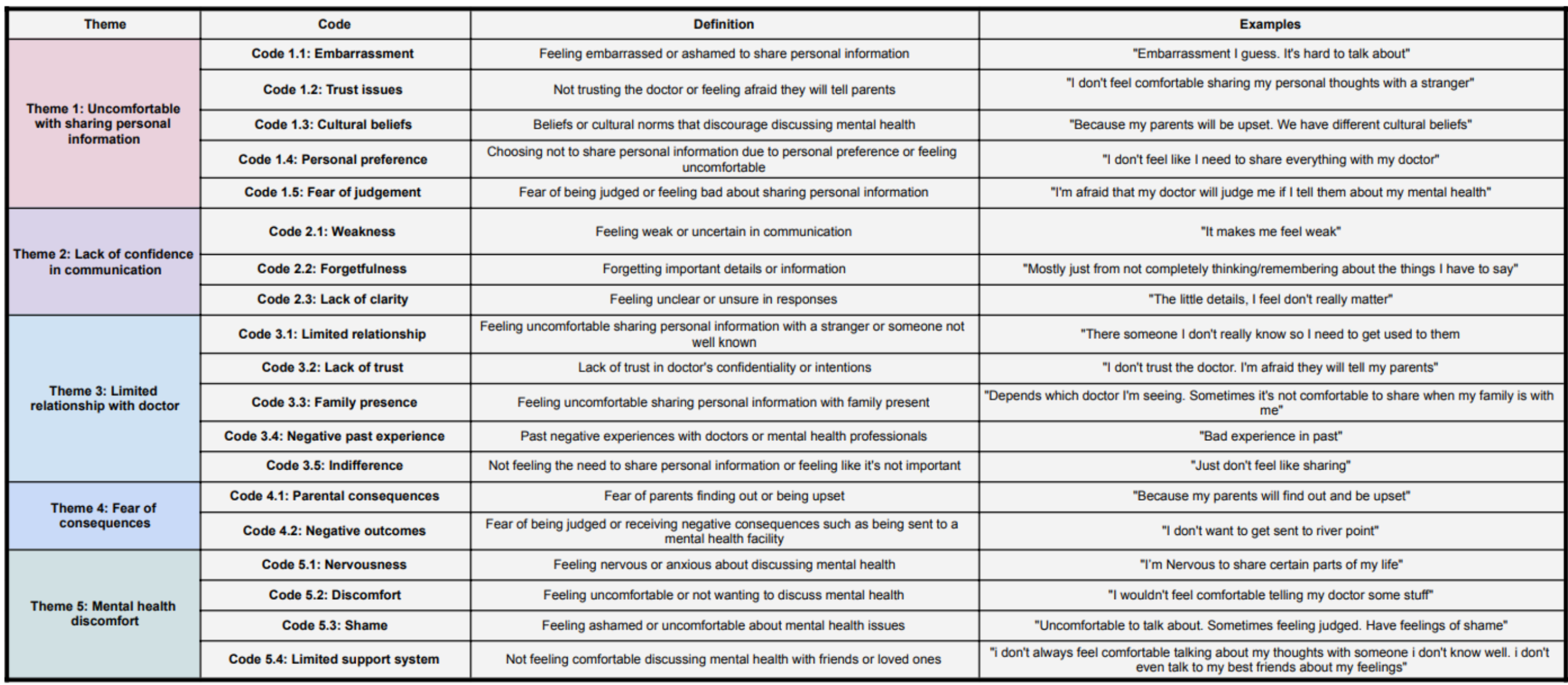
Results: We surveyed adolescents (12-19 years old: 54 females, 44 males, 3 non-binary) and pediatric physicians (60 females, 35 males, 5 undisclosed) to determine preferences in doctor-patient communication. Most adolescents trust their physician but refrain from seeking help for anxiety and depression (Table 1). Challenges in discussing MH, sexual activity, and drug use persist due to discomfort, fear, and lack of confidence (Table 2). Adolescents often withhold or provide false information (98%). Physicians also encounter discomfort discussing sensitive topics, facing barriers such as trust, confidentiality, parental presence, time constraints, stigma, and unease. 50% of adolescents prefer digital interactions, while 78% of physicians favor F2F. We also assessed comfort in sharing and obtaining MH information via a virtual reality (VR) avatar; 65% of teens felt comfortable with VR and 25% remained neutral, while only 35% of physicians were comfortable with this method.
Conclusion(s): This study aligns with previous studies identifying barriers to communication regarding MH. A novel finding is the disconnect between physicians and adolescents regarding preference for digital versus F2F interactions when discussing sensitive topics. Future research is needed, as closing this gap is vital to improving healthcare services and better meeting the MH needs of adolescents.