Emergency Medicine
Session: Emergency Medicine 10: Trauma
395 - Does Improving Timely Pain Assessments Drive Increased Pain Treatment with Opiates for Pediatric Patients with Long-bone Fractures?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 395
Publication Number: 395.2823
Publication Number: 395.2823

Israel Green-Hopkins, MD (he/him/his)
Director of Quality and Safety, Pediatric Emergency Medicine
UCSF Benioff Children's Hospital, San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Timely analgesia for patients with long-bone fractures (LBFs) in emergency departments can be dependent on documentation of pain assessments. Our institution recently improved our rates of pain assessment from a state of wide variation to minimal variation through a multidisciplinary quality improvement effort. The effect of improving assessments on choice of analgesics is unknown, and necessary to determine good opiate stewardship for patients with LBFs.
Objective: We sought to determine whether the decreased variation in pain assessments was associated with increased rates of opiate use for patients with LBFs in initial moderate to severe pain.
Design/Methods: We performed a retrospective cohort study and included patients ages 0-18 years treated for LBFs. We examined pharmacologic analgesia rates for patients in initial moderate to severe pain pre-intervention (01/2018-11/2019, 54% of patients had initial pain assessment within 30 minutes) and post-intervention (02/2020-02-2022, 80% of patients had initial pain assessment within 30 minutes). We included all patients whose initial pain assessment occurred within 90 minutes of arrival. Our primary outcome was receipt of any pharmacologic analgesia within 90 minutes of ED arrival, which could occur up to 30 minutes before or 60 minutes after the initial pain score. Our secondary outcome was time to analgesia in minutes. We analyzed differences using t-test for continuous variables and Chi-Square test for categorical variables.
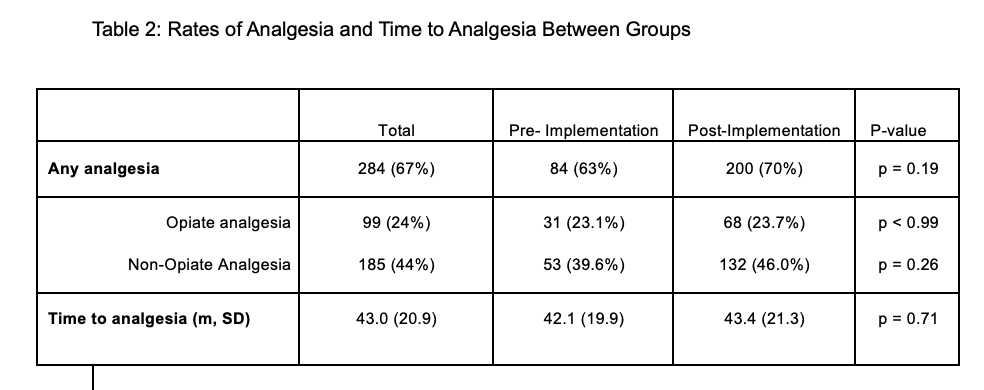
Results: During the pre-intervention period, 134 patients (median age=8.5y (6,12), 60% male) were included; during the post-intervention period, 287 patients (median age=8y (6,12), 56% male) were included (Table 1). There were no significant differences in receipt of pharmacologic analgesia between the groups (Table 2, 63% vs. 70%, p=0.19). There were no differences in the rate of opiate analgesia (23% vs. 24%, p< 0.99) or non-opiate analgesia between the pre and post-intervention periods (40% vs. 46%, p=0.26). The mean [SD] time to any pharmacologic analgesia was not different between pre and post-intervention periods (42 [20] minutes vs 43 [21] minutes), p=0.71).
Conclusion(s): Our analysis demonstrates that improvement in timely pain assessment for children with LBFs did not translate to increased rates of opiate or non-opiate analgesic use, suggesting that opiate stewardship was not affected by improved timely pain assessment. Further investigation into factors impacting analgesia administration and documentation of nonpharmacologic analgesia are important next steps.
.png)