Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 3
509 - Knowledge of Resuscitation Alone without Skills Feedback is Insufficient for Bag Mask Ventilation Proficiency in Tanzania
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 509
Publication Number: 509.560
Publication Number: 509.560

Emily Ahn, MD (she/her/hers)
Assistant Professor of Pediatrics
Weill Cornell Medicine
New York, New York, United States
Presenting Author(s)
Background: Basic knowledge of resuscitation physiology and technical skills are essential for the management of a nonbreathing infant at birth. Currently, at Kilimanjaro Christian Medical Centre in Tanzania midwives are the primary birth attendants with an inconsistent pediatric resident (PR) presence.
Objective: Assess resuscitation knowledge and bag mask ventilation (BMV) skills in PR and midwives.
Design/Methods: PR and midwives were given a 15-question multiple-choice knowledge test adapted from the Helping Babies Breathe program with the addition of technical BMV questions. Participants underwent BMV assessment utilizing the NeoNatalie Live trainer and NeoBeat (Laerdal Medical). BMV skills were scored on head positioning, inflating pressure (20-30 mmHg), rate (40-60 bpm), and maintenance of heart rate >100 bpm as measured by the manikin. Manikin heart rate response is linked to effective ventilation. Data analysis included t-test and chi-squared.
Results: Participants included 16 midwives and 16 PR. The percentage of PR vs midwives who answered ≥80% of knowledge questions correctly (75% vs 69%, P=0.69) was similar, as were the mean scores (12.75 ± 1.69 vs 11.69 ± 2.06, P=0.12). The most commonly missed questions for PR were infant response to unnecessary suctioning indicating they suction to increase the baby’s heart rate and starting BMV inflating pressure. The most commonly missed questions for midwives were goal BMV rate and infant response to unnecessary suctioning indicating they use it to cause the baby to cough and breathe (Table 1).
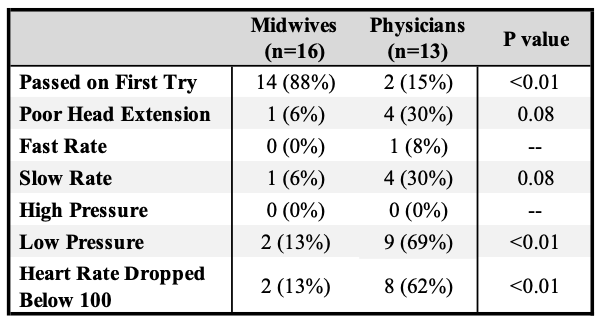
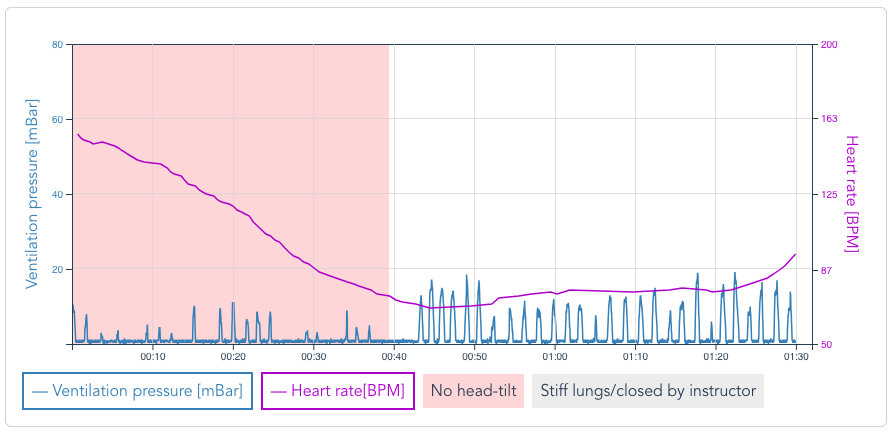
BMV data from the Live Trainer demonstrated that midwives were significantly more likely to meet all BMV criteria on the first attempt (88% vs 15%, P< 0.01, Table 2). More PR than midwives started ventilation with low initial inflating pressures (69% vs 13%, P< 0.01) presumed to be from mask leak and more PR had the manikin heart rate drop below 100 (62% vs 13%, P< 0.01) due to obstruction or inadequate pressures. With trainer feedback (Fig 1), all participants met BMV requirements after varying attempts.
Conclusion(s): Knowledge of neonatal resuscitation alone did not translate into delivery of adequate BMV skills as both PR and midwives scored well on knowledge testing but only midwives performed well on BMV assessment. An important knowledge gap is why and when to use suctioning. NeoNatalie Live provides immediate visual provider feedback highlighting areas for improvement. This facilitates the participant’s ability to master BMV skills with repeated attempts in a non-threatening environment. Next steps include repeat BMV testing over time to assess skills retention.
.png)
