Neonatology
Session: Neonatal Quality Improvement 1
384 - Improved Discharge Weight in Preterm Infants with a Comprehensive Small Baby Program and Nutritional Care Bundle
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 384
Publication Number: 384.2222
Publication Number: 384.2222

Julianna Diddle, MD (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Dedicated small baby programs have been shown to improve survival and other outcomes in extremely preterm infants. Our level III NICU transitioned to a new medical provider team in July 2021 and launched a small baby program (SBP) in January 2022. After needs were assessed, three key drivers were implemented: educating a core multidisciplinary team, securing a dedicated space, and applying evidence-based standardized guidelines for infants born less than 27 weeks gestational age (GA) or 800 grams birth weight (BW). Extrauterine growth restriction was addressed by implementing a nutritional care bundle that includes an enteral feeding and nutritional supplement protocol. The key drivers and processes of our SBP are described in figure 1.
Objective: The overall objective of the SBP is to improve survival without major morbidities. A secondary objective is to increase the proportion of infants with discharge weight >10th percentile.
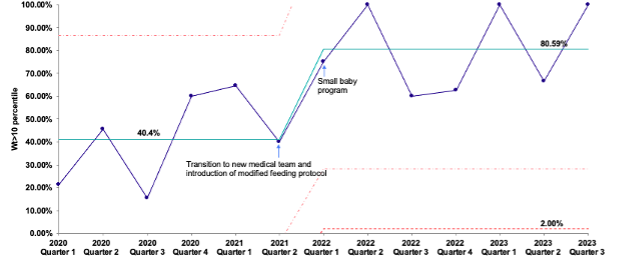
Design/Methods: As part of a quality improvement initiative, we prospectively collected data on maternal-infant characteristics, and process and outcome measures including discharge weight percentile. Baseline data for 18 months prior to the transition of the medical team (January 2020-June 2021) and after the launch of the SBP (January 2022-September 2023) were obtained retrospectively from our center’s VON data. A statistical process chart was used to analyze the proportion of infants discharged at weight >10th percentile quarterly, at baseline and post-SBP implementation.
Results: A total of 209 infants were included in the study. 98 infants with birth GA less than 27 weeks or BW less than 800 grams were admitted in the baseline cohort, of which 75 (76.5%) were discharged home from our center. 111 infants were admitted in the post-SBP cohort, of which 84 (75%) infants were discharged home excluding deaths, transfers and currently admitted patients. The median GA, birth weight, and proportion of infants with birth weight below the 10th percentile were not different between the baseline and SBP cohorts (Table 1). The percentage of infants discharged home with weight above the 10th percentile was 40.4% in the baseline cohort and increased to 80.59% in the SPB cohort (Figure 2).
Conclusion(s): We described our early experience of a small baby program with a comprehensive nutritional bundle and report an increase in the proportion of infants with discharge weight above the 10th percentile in comparison to baseline data. Continued monitoring of process and outcome measures are needed to evaluate the long-term impact of the small baby program.
.png)
.png)
