Neonatology
Session: Neonatal Quality Improvement 6
91 - Implementation of the NICU “Golden Hour” – A Quality Improvement Project for Preterm Infants
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 91
Publication Number: 91.2786
Publication Number: 91.2786

Morgan F. Smith, DO (he/him/his)
Pediatric PGY-2 Resident Physician
Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine
Honolulu, Hawaii, United States
Presenting Author(s)
Background: Prematurity remains the leading cause of neonatal and childhood morbidity and mortality in the United States and developed world with increasing rates of death or health complications directly correlating to degree of prematurity and lower birth weights. The NICU “Golden Hour” refers to a series of team-oriented, task-driven evidence-based interventions applied during the initial hours of life with the goal of improving both short term and long-term outcomes. Utilizing these principals, our team aims to improve efficacy and standardization of our NICU admissions process.
Objective: Our primary objective was to standardize interventions and initial care of very preterm and very low birthweight newborns. Secondary objectives were to decrease time to interventions such as time to IV fluid administration and time to first dose of antibiotics. We also aimed to improve time from delivery room to NICU, and to reduce hypothermia rates at both admission and one hour.
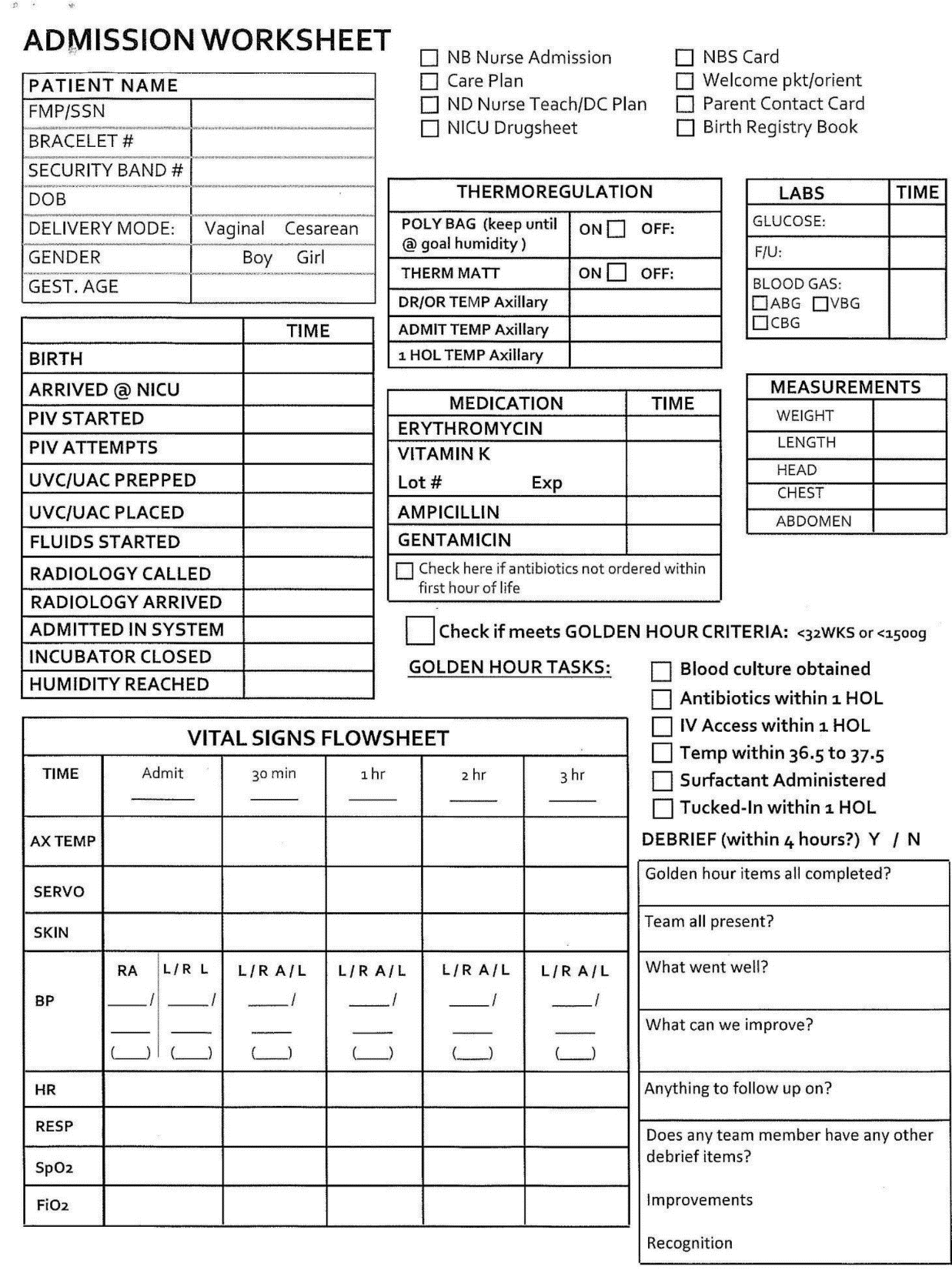
Design/Methods: The Golden Hour protocol was implemented in February of 2021. All infants with an estimated gestational age less than 32 weeks and/or a birthweight of less than 1500 grams met inclusion criteria. There was no exclusion criteria. A standardized order set was created for admissions. Frequent in-service meetings and education was provided to all levels of the care team in the NICU. Times to interventions were tracked on a flow sheet.
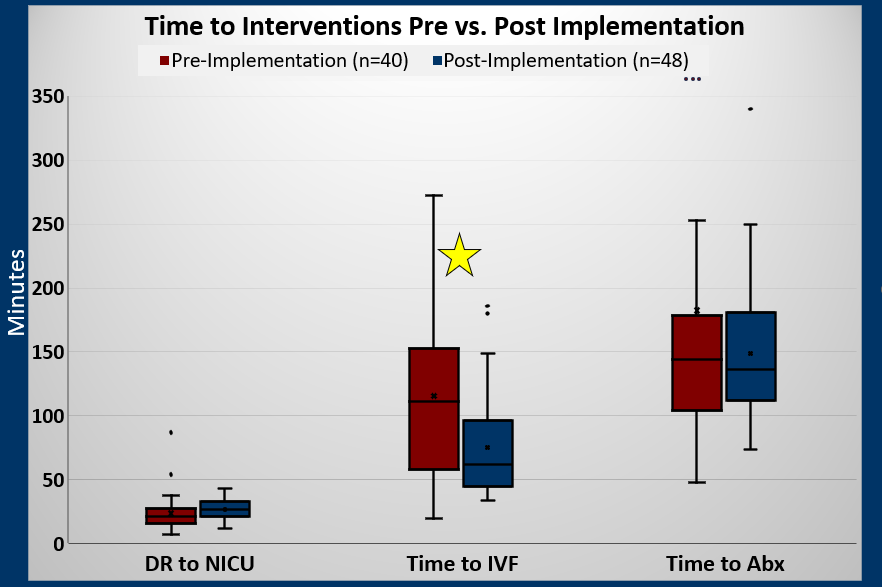
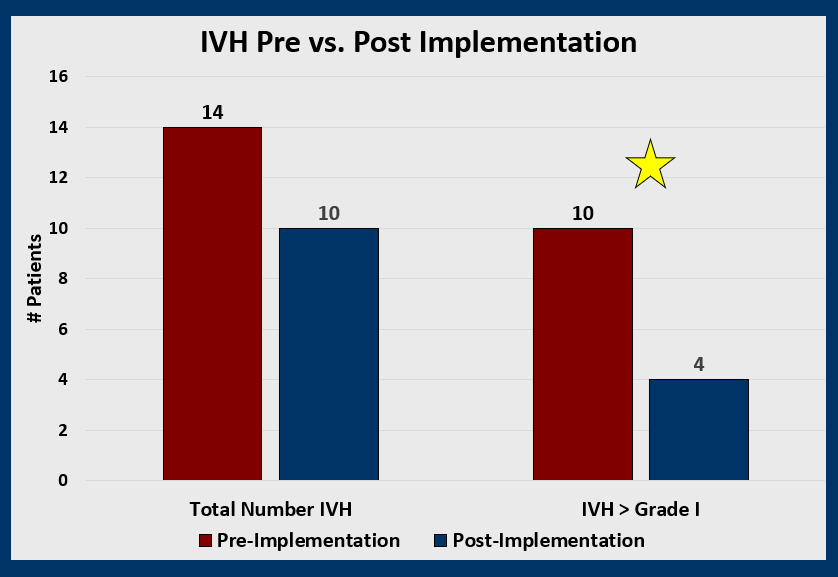
Results: The pre (n=40) and post-implementation (n=55) cohorts showed no statistical differences in sex, birthweight, gestational age, or route of delivery. Post-protocol group had a decreased rate of maternal antenatal steroid administration (92% vs 73%, p=0.031). We saw no difference in time to starting antibiotics. There was a decrease in time to intravenous fluids from 115.5 to 73.2 minutes (p=0.0005), and increased time from birth to NICU admission, 23.6 to 26.3 minutes (p=0.0087). Patient temperature did not change. When looking at rates of intraventricular hemorrhages we saw a significant reduction in rates of clinically significant IVH (grades 2-4) with an OR of 0.14 [95% CI 0.03-0.717] post-protocol.
Conclusion(s): While implementation of our protocol did not result in differences in time to antibiotics or admission temperatures, it was associated with statistically significant decreases in time to intravenous fluids administration and rates of clinically significant IVH. These results suggest that the standardization of care and attention to early intervention in very low birth weight and very premature infants results in significantly improved health outcomes.