Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
474 - Association of Enteral, Parenteral, and Total Fluid Volumes in First Week with In-Hospital Outcomes among Premature Newborns in a Tertiary Referral Hospital in Addis Ababa, Ethiopia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 474
Publication Number: 474.581
Publication Number: 474.581

Olivia C. Brandon, BS (she/her/hers)
Research Scientist
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: The ideal balance of enteral feeds (EF) to parenteral fluids (PF) for preterm newborns remains unclear. Increasing total fluid intake (TFI) is associated with adverse in-hospital outcomes such as necrotizing enterocolitis (NEC), although studies lack granularity in assessing the relative contribution of EF and PF. As >98% of all deaths due to prematurity occur in low- and middle-income countries, research is especially needed in these settings.
Objective: To evaluate the association between EF, PF, and TFI in the first week after birth with in-hospital morbidity and mortality among premature newborns in a large tertiary referral hospital, St. Paul’s Hospital Millennium Medical College (SPHMMC) neonatal intensive care unit (NICU), in Addis Ababa, Ethiopia.
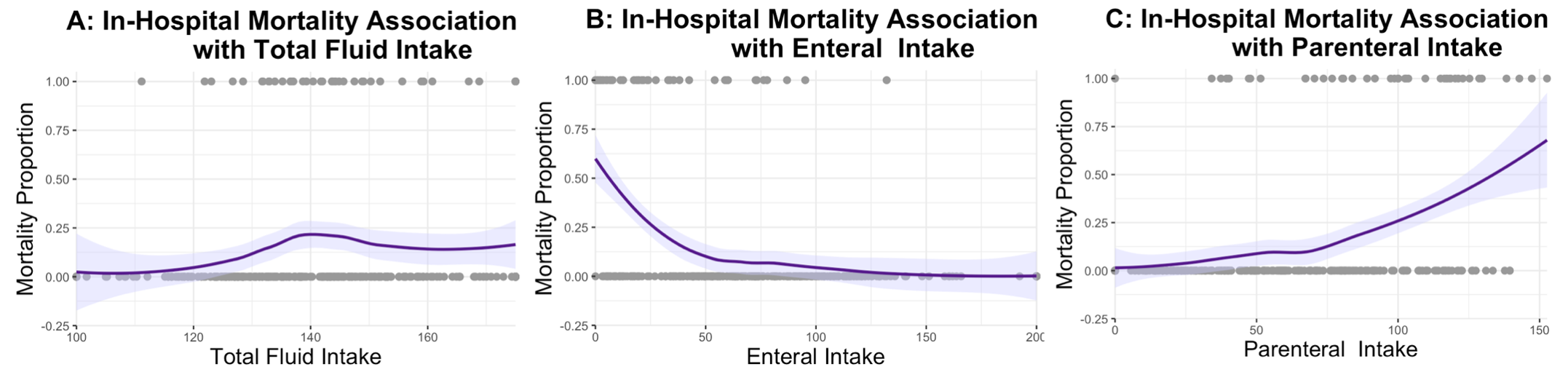
Design/Methods: We conducted a prospective cohort study among newborns born < 37 weeks’ gestation who survived and remained in hospital for one week after birth with complete fluid intake and weight data. We used continuous curves of fluid intake and in-hospital mortality where the 95% CI did not include 0% to determine categorical cut-off values for EF, PF, and TFI analyses. Logistic regression models assessed fluid intake (EF, PF, and TFI) and association with in-hospital mortality after the first week, necrotizing enterocolitis (NEC), sepsis, retinopathy of prematurity (ROP), and length of hospital stay (LOS).
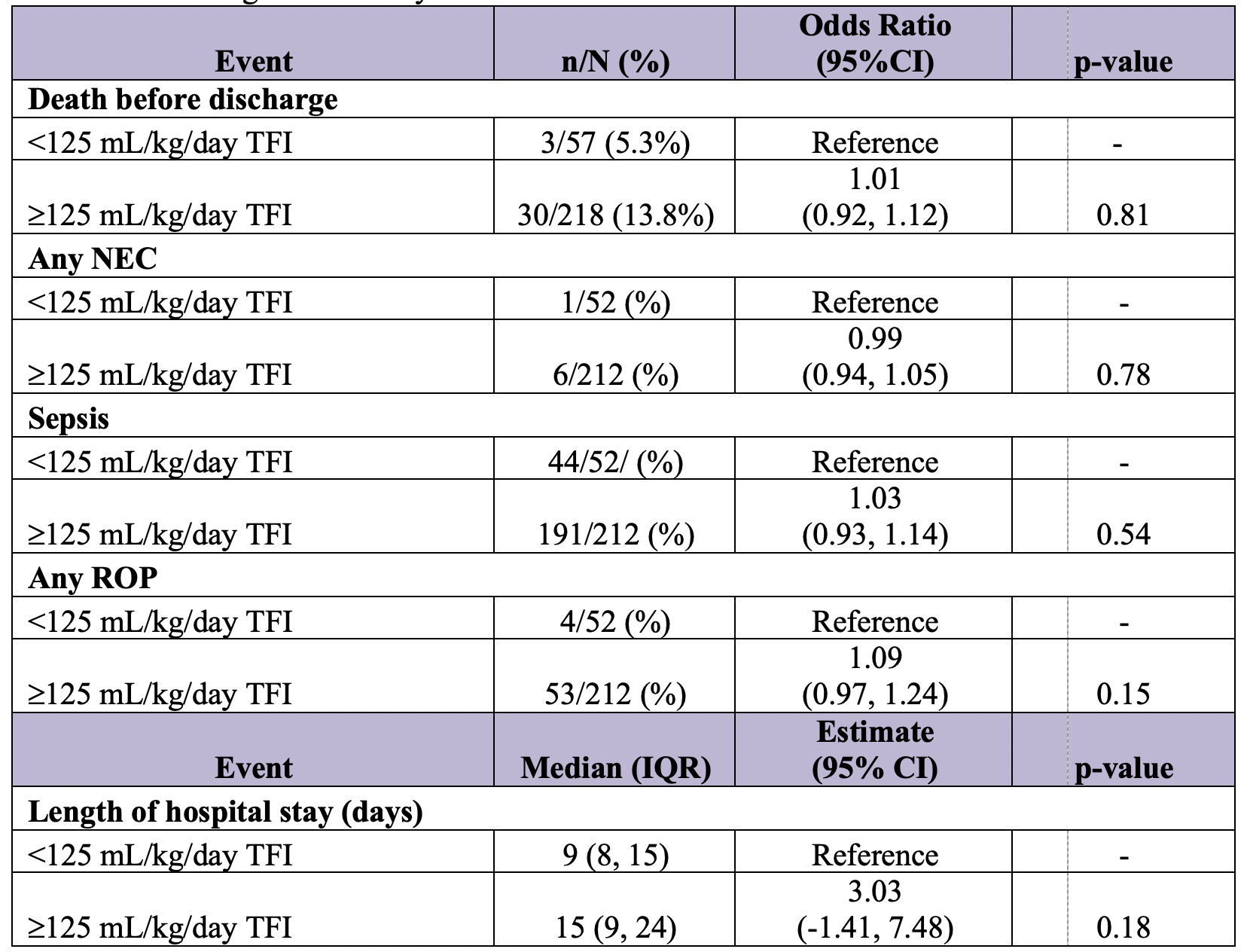
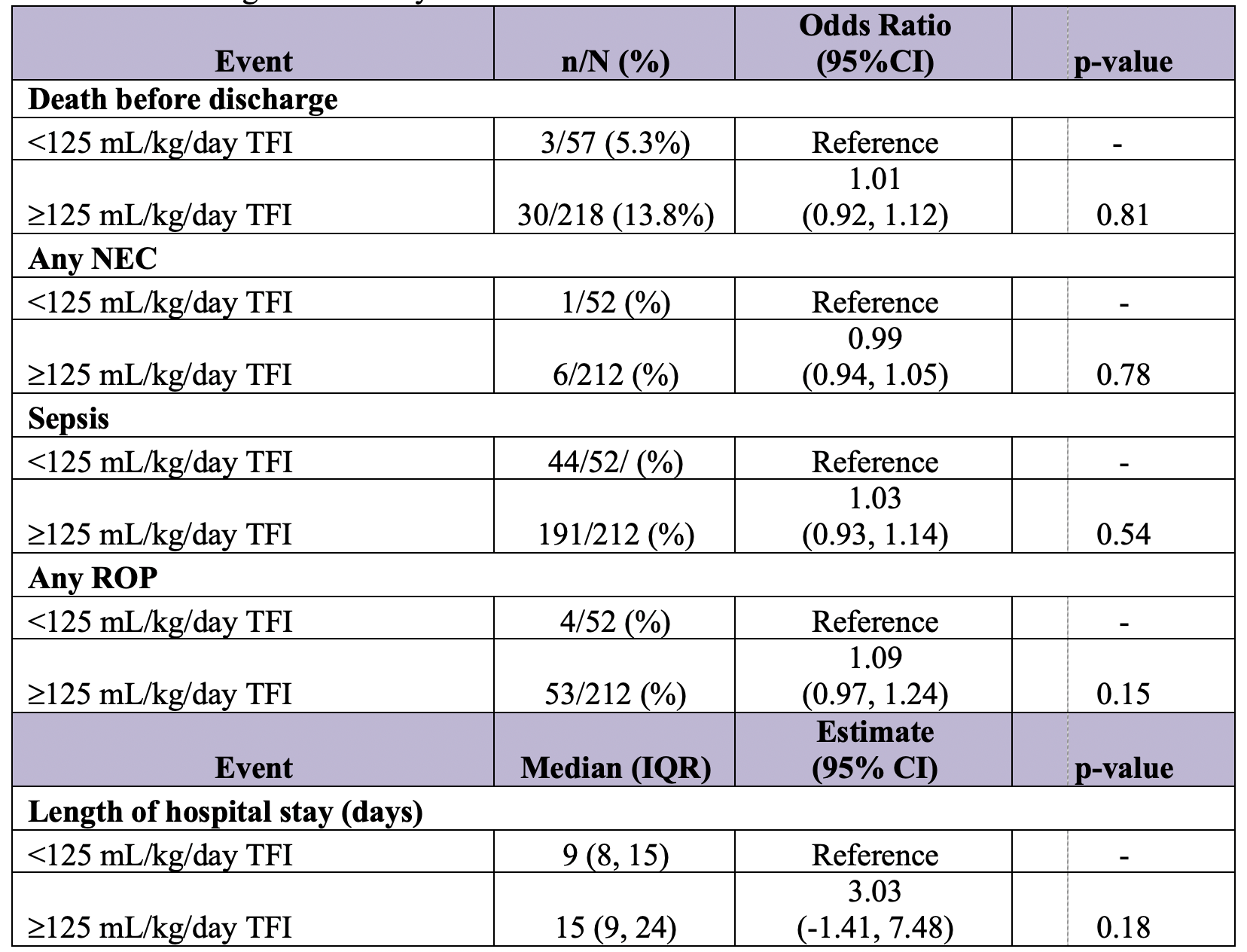
Results: Among N=275 preterm infants who survived ≥1 week after birth and had complete fluid intake and weight information, mortality proportion was reduced as EF increased and PF or TFI decreased (Figure 1). After adjusting for potential confounders, infants who received ≥125 mL/kg/day average TFI in the first week did not have increased odds of in-hospital morbidity or mortality (Table 1). Those who received ≥50 mL/kg/day average EF in the first week had 12% reduced odds of in-hospital mortality (adjusted OR 0.88, 95% CI 0.79, 0.98; Table 2) and a significantly shorter hospital stay (8.55 fewer hospitalized days, 95% CI -13.6, -3.45) compared to those who received < 50 mL/kg/day EF. Average PF 50 mL/kg/day was not associated with in-hospital adverse outcomes.
Conclusion(s): While neither TFI nor PF intake were associated with adverse outcomes, increasing EF, especially ≥50 mL/kg/day in the first week after birth, was associated with reduced odds of in-hospital mortality and a shorter hospital stay among preterm newborns. Future efforts are needed to increase EF volumes among preterm newborns at SPHMMC NICU.