Critical Care
Session: Critical Care 1
109 - Improving Fluid Overload Among Critically Ill Children: Federated Data Analysis for Multi-Center Quality Improvement
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 109
Publication Number: 109.2767
Publication Number: 109.2767

Adam Dziorny, MD, PhD
Assistant Professor, Pediatrics & Biomedical Engineering
UR Medicine Golisano Children's Hospital
Pittsford, New York, United States
Presenting Author(s)
Background: Fluid overload (FO), a state of pathologic % cumulative fluid balance (%CFB), is common in children with critical illness and associated with increased length of stay (LOS), morbidity, and mortality. Multisite quality improvement (QI) partnerships allow for sharing strategies to potentially reduce FO. To lower the barrier to automated data extraction, we can apply a federated data collection framework to leverage single center informatics expertise. This framework does not rely on data sharing, but rather includes local analysis with central result aggregation. We apply this novel paradigm to a QI study to reduce FO in the pediatric intensive care unit (ICU).
Objective: We aim to use a federated data collection framework to generate pre-intervention FB metrics at 3 PICUs in preparation for a multi-site QI project to decrease %CFB.
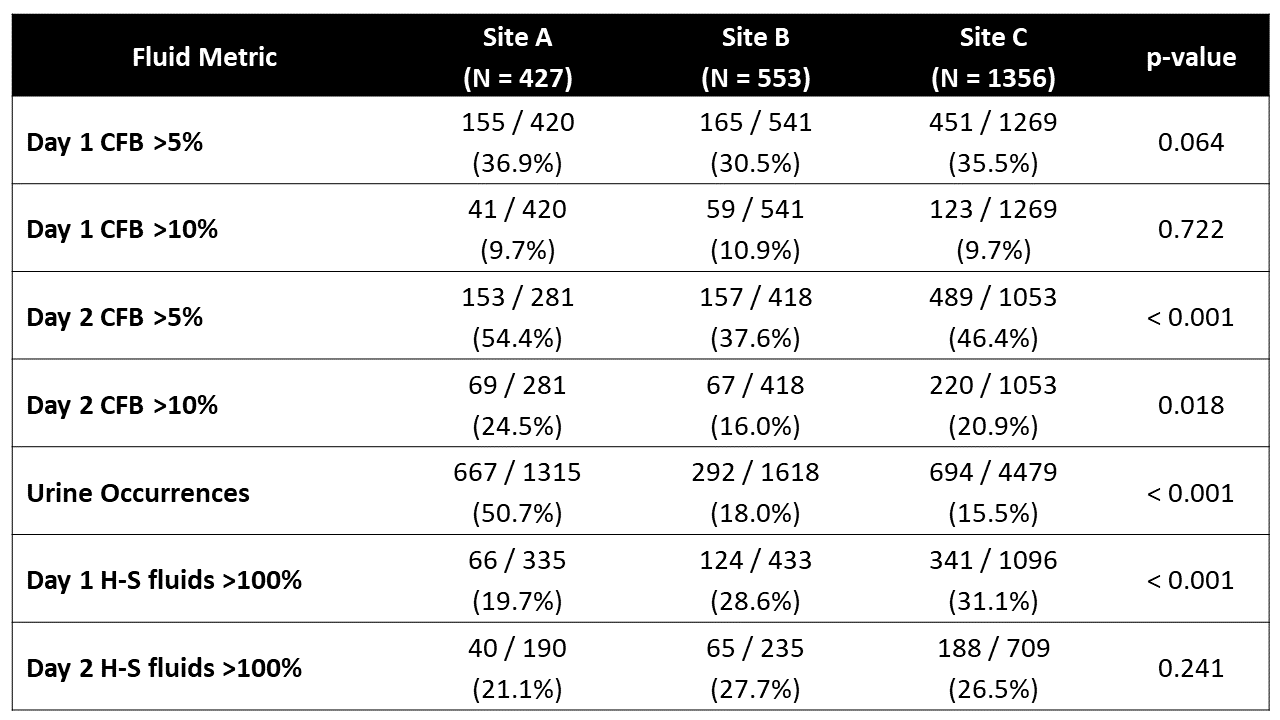
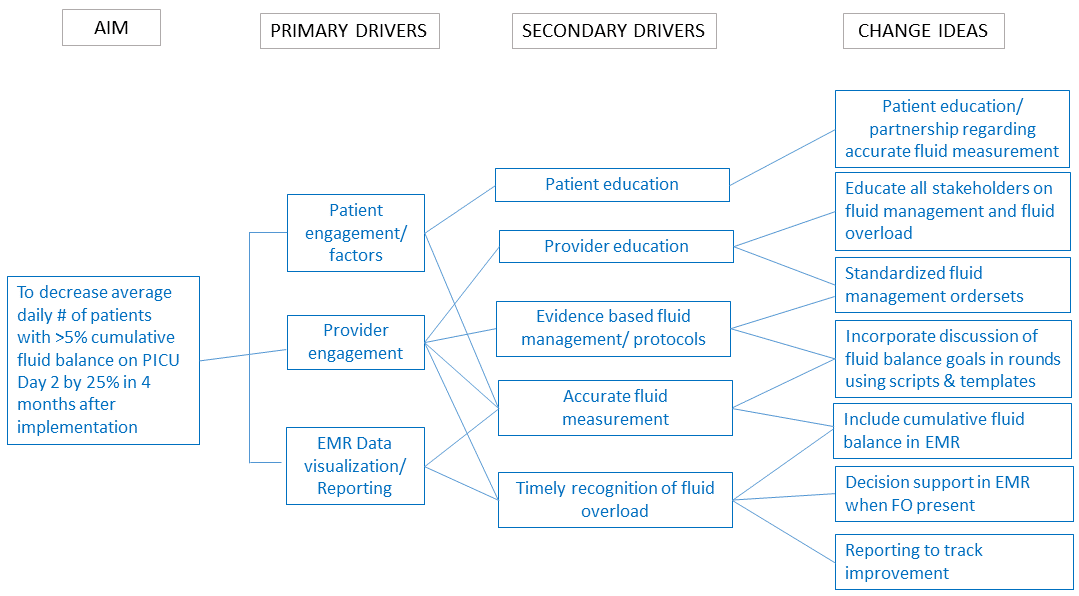
Design/Methods: All participating sites utilize the same electronic medical record. After identifying the key drivers of positive %CFB in the ICU (Figure 1), we developed a SMART Aim and identified key metrics including: baseline demographics, %CFB (intake minus output normalized to weight), urine occurrence counts, relationship to Holliday-Segar (H-S) maintenance fluid rates, and associations with mechanical ventilation and ICU LOS. Analysis scripts were written at a single site and run locally at individual sites. Results were aggregated and reviewed centrally. Chi-square test and Wilcoxon rank sum were used to compare results across and within sites.
Results: Over a 6-month period we included 2336 ICU encounters encompassing 1984 children. Mean number (%) of patients with day 2 CFB >5% significantly differed by site (A: 153 (54.4%), B: 157 (37.6%), C: 489 (46.4%); p< 0.001; Figure 2 & Table 1). Mean number of patients with urine occurrences and number of patients receiving >100% of H-S fluids on day 1 differed by site (Table 1, p < 0.001 for each). Mechanical ventilation orders were associated with receiving >100% of H-S fluids on day 1 and day 2 at each site (A: 28.5% vs 13.3%; B: 40.3% vs 23.7%; C: 49.8% vs 23.4%) and (A: 25.0% vs 15.4%; B: 34.0% vs 23.4%; C: 43.0% vs 15.8%), respectively. Days 1 and 2 CFB >5% was significantly associated with increased ICU LOS at each site (p < 0.001).
Conclusion(s): Using a federated data collection framework, we demonstrate positive %CFB is a common but variable problem across 3 PICUs. Results of our work have identified areas for improvement that will inform PDSA cycles for next steps of this project.
.png)