Neonatology
Session: Neonatal Follow-up 3
537 - Impact of the COVID-19 Pandemic on Developmental Outcomes in Infants Treated with Therapeutic Hypothermia
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 537
Publication Number: 537.2755
Publication Number: 537.2755

Sriya Roychaudhuri, MD, MRCPCH (she/her/hers)
Clinical Assistant Professor
University of British Columbia Faculty of Medicine
Vancouver, British Columbia, Canada
Presenting Author(s)
Background: The pandemic disrupted the social structure and medical services and compounded the stress in families of hospitalized infants. Incidence and management of newborn encephalopathy (NE) benchmark healthcare practices. Infants with NE who undergo therapeutic hypothermia (TH) are vulnerable to brain injury, yet developmental outcomes in this population during the pandemic remain unknown.
Objective: To assess the impact of Covid-19 pandemic and family-social risk on early neurodevelopment of infants with NE.
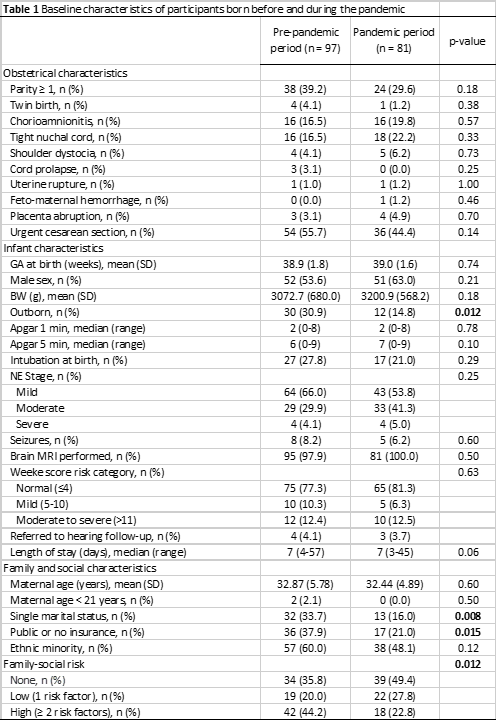
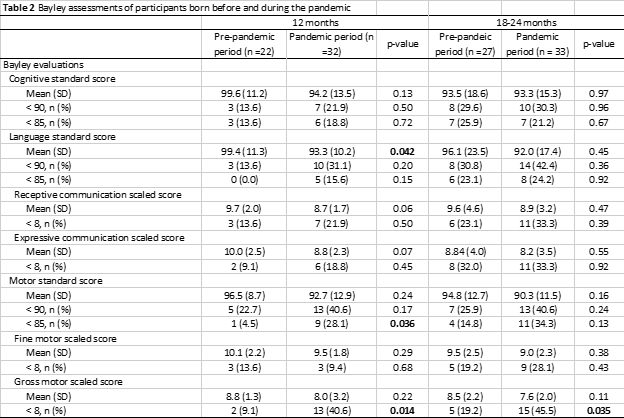
Design/Methods: We conducted a retrospective review of infants treated with TH for NE in a level 3 center. We compared outcomes of infants born during the pandemic, from 03/2020–09/2021, to infants born before, from 10/2017–12/2019. Neurodevelopmental outcomes were assessed using the Bayley Scales of Infant Development 4th edition (BSID-4) at 12 months and at 18-24 months corrected age. Baseline demographic data were retrieved, and post-rewarming MRIs were scored for injury. We assessed associations of developmental outcomes relative to the pandemic period using t-tests and chi-square tests and examined the impact of high family-social risk (≥2 risk factors including maternal age < 21 years, single marital status, public or no insurance, and ethnic minority) graphically.
Results: There was no significant difference between perinatal characteristics and baseline severity of injury due to NE in the two cohorts (Table 1). However, the pre-pandemic cohort appeared to experience increased family-social risk (p=0.012). Compared with the pre-pandemic period, infants treated with TH during the pandemic displayed lower language scores (93.3 vs 99.4; p=0.042) and more motor delays (28.1% vs 4.5%; p=0.036) at 12 months (Table 2). Gross motor impairments were more prevalent during the pandemic up to 24 months of age (45.5% vs 19.2%; p=0.035). ASQ and MCHAT scores were comparable. During the pandemic, the gap between language scores of infants from at-risk families compared to low-risk families appeared wider (Figure 1).
Conclusion(s): This study suggests that motor and language outcomes of infants treated with TH for NE may be impacted by the COVID-19 pandemic. The developmental differences despite similar healthcare delivery could possibly reflect limited access to care and post-discharge supportive services, increased family stress, and/or other social factors that may have been impacted by the pandemic. The findings highlight that infants from socially at-risk families may be especially vulnerable in periods such as the COVID-19 pandemic.
.jpg)
