Emergency Medicine
Session: Emergency Medicine 6: Airway and POCUS
197 - Point-of-Care Ultrasound Role in Ovarian Torsion to Expedite Confirmatory Testing (PROTECT): A Quality Improvement Initiative
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 197
Publication Number: 197.2197
Publication Number: 197.2197

Sonali Bhalodkar, MD, MPH (she/her/hers)
Clinical Fellow, Pediatric Emergency Medicine
Yale-New Haven Children's Hospital
New Haven, Connecticut, United States
Presenting Author(s)
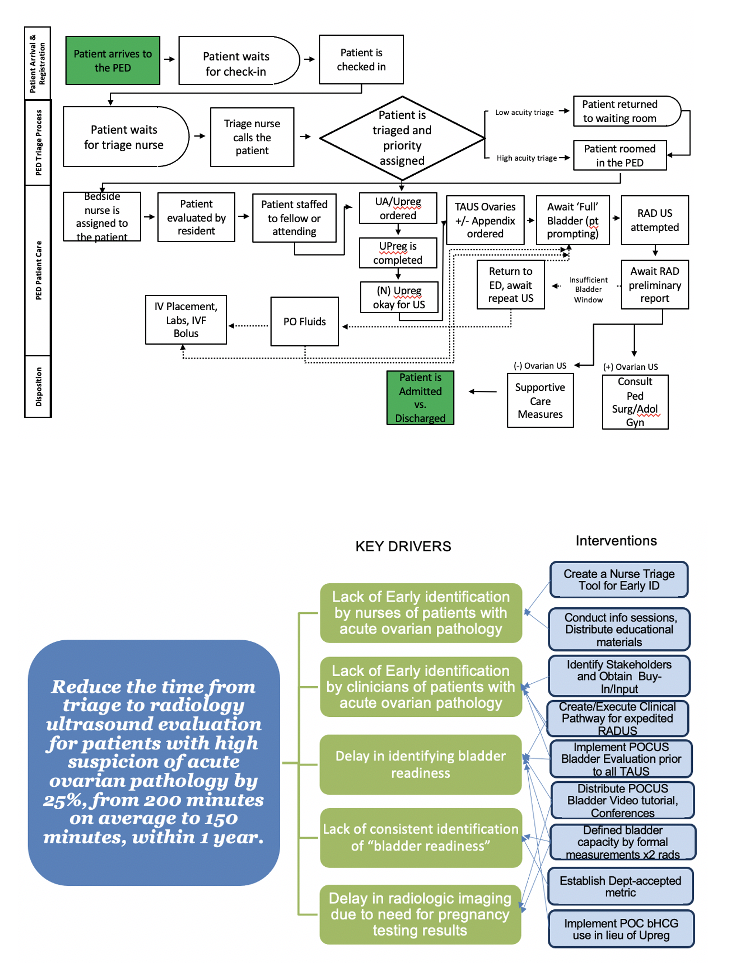
Background: Early identification and management of acute ovarian pathology, including pediatric torsion, can prevent gonadal loss, improve outcomes and decrease health care expenditures. The many challenges to early diagnosis of female gonadal emergencies contribute to inequitable care, and bedside ultrasound may be a tool to remedy this.
Objective: The global aim is to improve equitable care for females with undifferentiated genitourinary emergencies. The SMART aim of this QI project was to expedite the triage to radiology (TtRT) time for females in the pediatric emergency department with suspicion for acute ovarian pathology by 25% from July 2022 to February 2023. The primary outcome measure was the effect of POCUS on TtRT over the eight-month period. The secondary aim was to increase provider use of point-of-care ultrasound within our group.
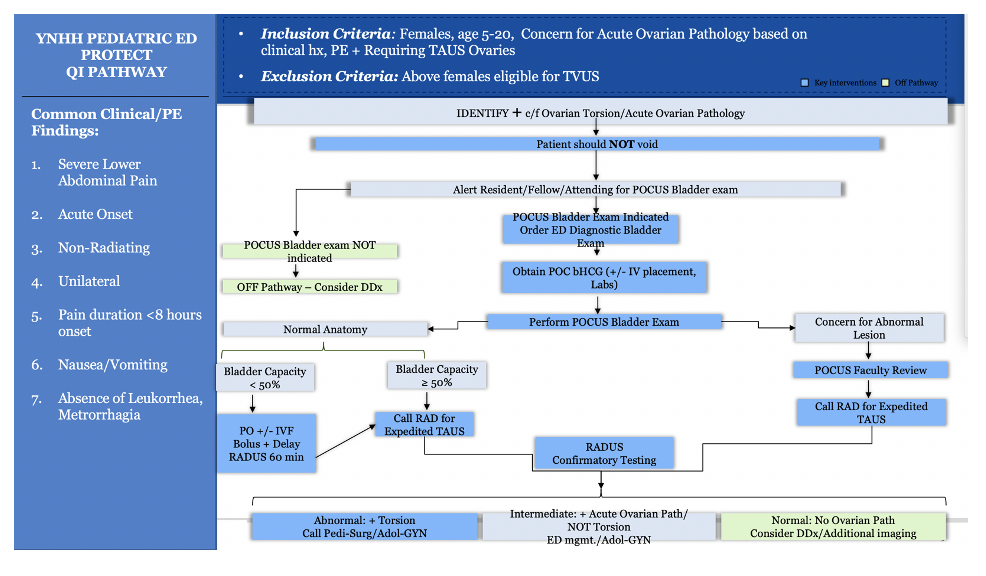
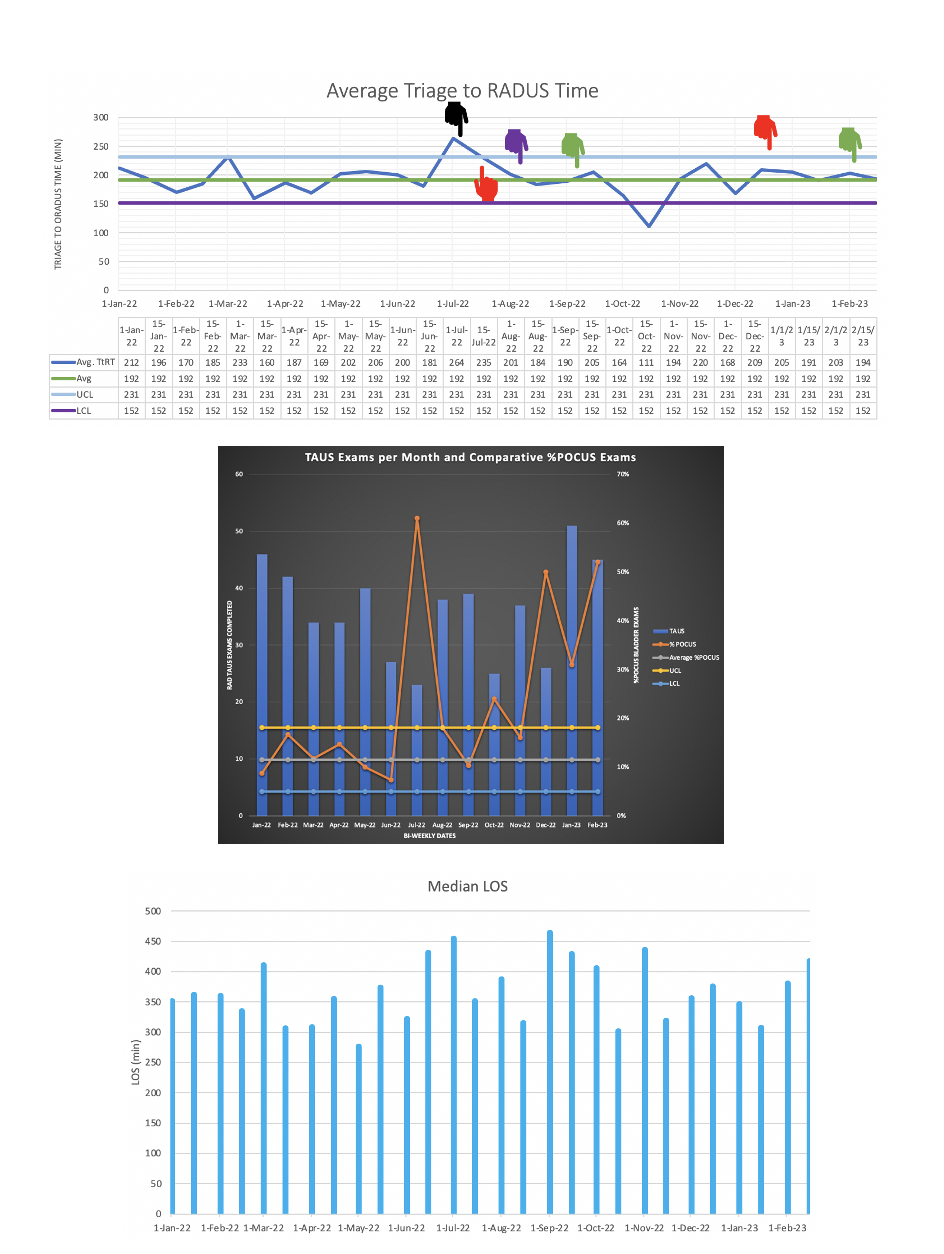
Design/Methods: This QI initiative, conducted at a single, quaternary care hospital pediatric emergency department utilized a multi-intervention process through PDSA cycles in an iterative change process. POCUS bladder exam was conducted to establish ‘bladder readiness,’ defined as 50% bladder capacity for age, for expedited radiology transabdominal pelvic ultrasound. Data was plotted on an interrupted time series control chart with additional p charts for secondary outcomes.
Results: Female patients age 5 to 20 years with suspected gonadal emergency undergoing transabdominal pelvic ultrasound were evaluated. Pre-intervention baseline characteristics for 223 patients were obtained from January 2022 through June 2022. Post-intervention outcomes for 284 patients were reviewed prospectively from July 2022 through February 2023. There was no significant change in Triage to Radiology Testing (TtRT) time pre-intervention (192 minutes) and post-intervention (196 minutes). POCUS utilization was completed in 33% of patients, and 78% of exams found insufficient bladder volume to expedite radiology testing. However, we showed upward trend in the utilization of POCUS bladder evaluation by all providers, not only ultrasound faculty.
Conclusion(s): Further iterative, Level 3 and 4 interventions are required to effect sustainable change in our current process. However, POCUS to pelvis in females with severe lower abdominal pain is a safe, fast, equitable and potentially gonad-saving intervention all providers should consider adopting.