Asthma
Session: Asthma 2
194 - Resident-led Quality Improvement Initiative to Improve Environmental Assessment in Pediatric Asthma
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 194
Publication Number: 194.495
Publication Number: 194.495

Brienne C. Lubor, MD (she/her/hers)
Resident Physician
Weill Cornell Medicine
New York City, New York, United States
Presenting Author(s)
Background: Asthma is the leading cause of chronic disease in children. The National Institutes of Health (NIH) Expert Panel Report-4 guidelines emphasize environmental assessment and intervention for patients with asthma. Our resident practice affiliated with an academic medical center, serves publicly insured children with a high burden of asthma, but low rates of identifying environmental triggers and allergies which may contribute towards poor asthma control.
Objective: To increase the percentage of environmental screening at well-child visits for patients with indoor allergies, poorly controlled or persistent asthma to at least 50%, and to offer environmental interventions to 90% of patients with a positive screen by June 2024.
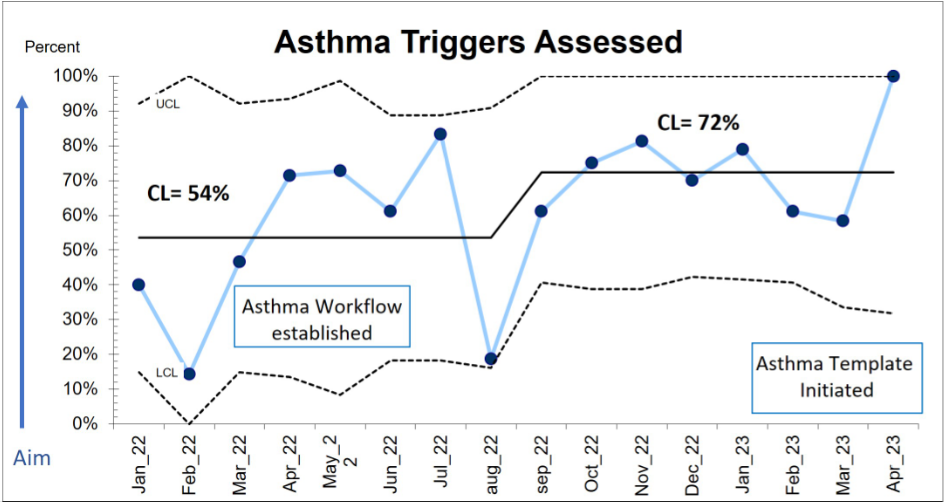
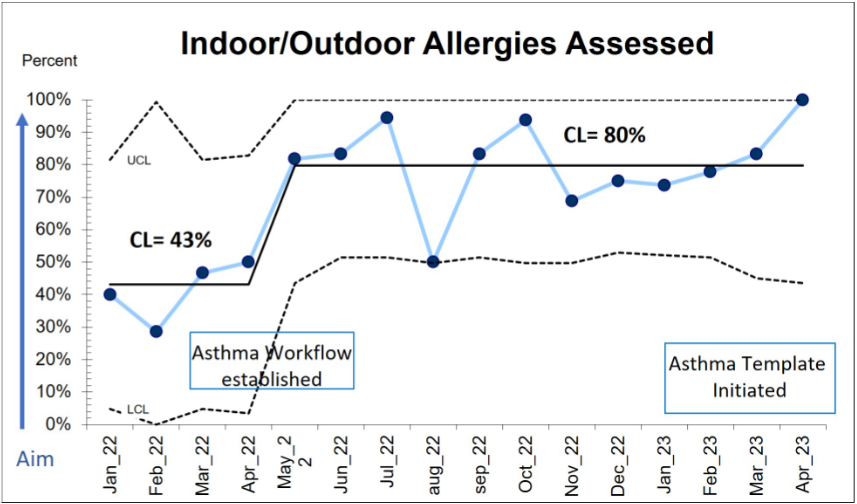
Design/Methods: This is an observational time series study with planned sequential experimentation from January 2022 to April 2023 using the Model for Improvement to design measures. Our main outcome measure was the receipt of interventions in patients with positive environmental screens. Process measures included the number of patients with documented asthma severity, control, indoor/outdoor allergies, and triggers during a clinic visit. Total clinic visit time was used as a balancing measure. Interventions were tested via several PDSA cycles including creation of a structured provider workflow, incorporating smart phrases into the Electronic Medical Record (EMR) to standardize documentation of asthma severity, control, allergies/triggers and environmental screens, and further refining an EMR template to automate that documentation. Statistical control “P” charts were used to display and analyze data. API rules were applied to detect special cause variation.
Results: In this study of 244 patients, we improved both assessment of indoor/outdoor allergies from 43% to 80%, and identification of triggers from 54% to 72% (Figures 1A and 1B). Asthma severity and control assessment remained stable at 90% (n =220) and 66% (n =162) respectively. Although environmental screening rate in the target population was at 15%, almost all were associated with an appropriate intervention. There was no change in total visit time.
Conclusion(s): We successfully improved rates of environmental allergy and trigger assessment, allowing for identification of patients who require intervention or additional services to improve asthma symptoms. The most successful interventions were introduction of a structured resident workflow and incorporation of required guideline-based elements into the EMR. Next steps include designing interventions to improve environmental screening rates.