Neonatology
Session: Neonatal General 1: NICU Care
47 - Clinical characteristics of neonates born less than 32 weeks gestational age to mothers with mental illness in an urban neonatal intensive care unit
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 47
Publication Number: 47.453
Publication Number: 47.453

Anya S. Alag, B.S. (she/her/hers)
Medical Student
USC Keck School of Medicine
Los Angeles, California, United States
Presenting Author(s)
Background: Studies have shown that maternal psychiatric illness negatively affects neonatal outcomes, including increased risk for preterm birth and poor fetal growth. Less is known about neonatal outcomes among very preterm infants born to mothers with mental illness. Our Level III neonatal intensive care unit (NICU) serves an underserved, urban population, positioning us to better study this important population.
Objective: Our objective was to evaluate maternal characteristics and outcomes of very preterm infants ( < 32 weeks) born to mothers with psychiatric conditions, in order to better understand the effects of maternal psychiatric history on fetal outcomes.
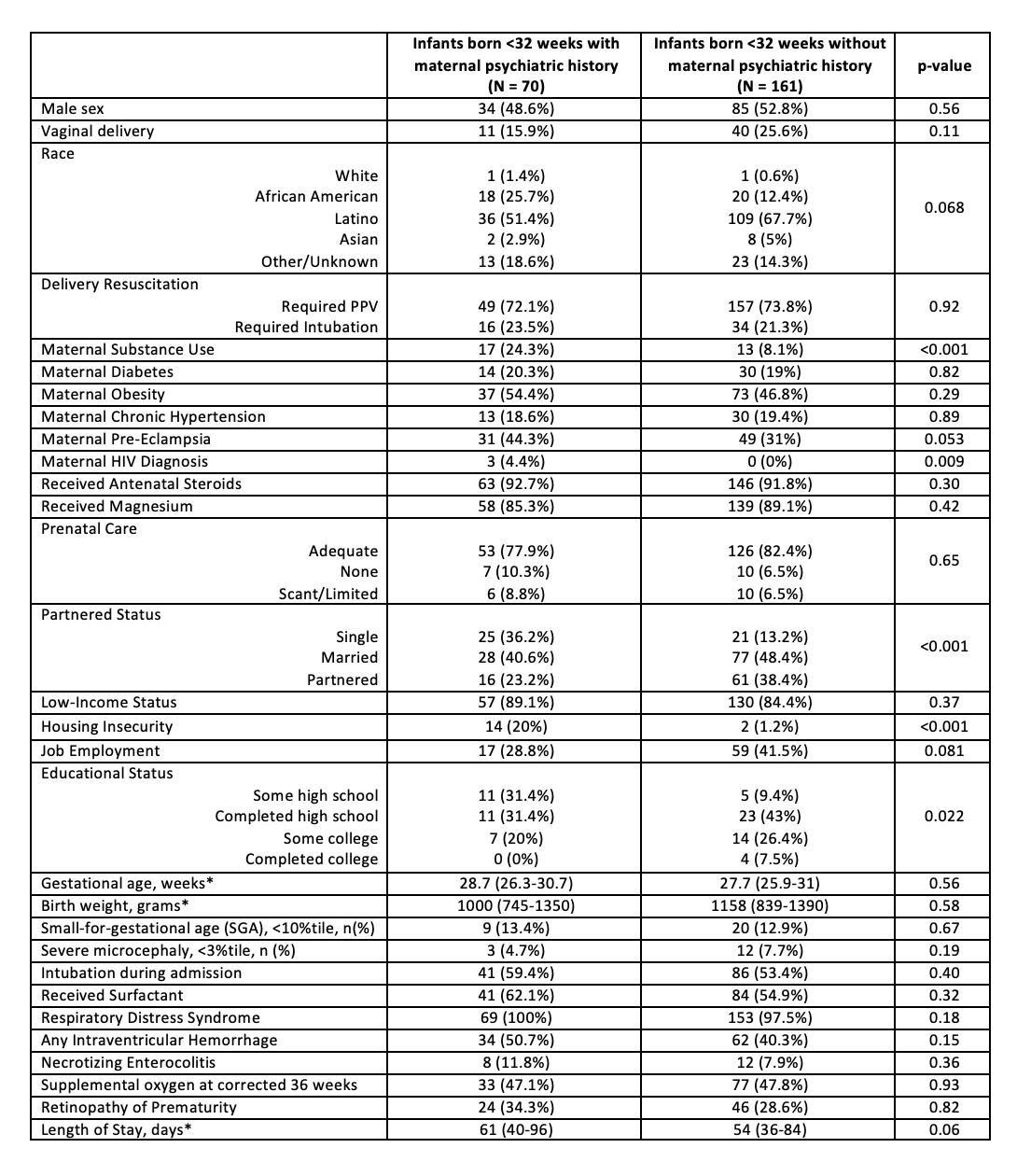
Design/Methods: We conducted a retrospective medical record review of neonates < 32 weeks gestational age admitted to an urban Level III NICU between 2017-2022. Maternal psychiatric illnesses were identified through physician documented diagnoses and maternal self-report in behavioral health and social work evaluations. Bivariate analyses were performed to assess maternal characteristics and neonatal outcomes for mothers with and without a psychiatric illness.
Results: A total of 231 neonates were identified, with 70/231 (30%) born to mothers with documented psychiatric illness history and 161/231 (70%) without a psychiatric diagnosis. Of the identified mothers with psychiatric history, 90% had a mood disorder diagnosis and 5.7% were diagnosed with both mood disorders and schizophrenia (Table). Predictors of maternal mental illness included single mothers, housing insecurity, and lower educational attainment. Maternal self-identified race, inadequate prenatal care, low-income status, and unemployment were not significantly different. Maternal psychiatric history was associated with HIV diagnosis but not other medical comorbidities, such as chronic hypertension, diabetes, obesity, and pre-eclampsia. Infants born to mothers with mental illness were not more likely to be small for gestational age or require delivery room resuscitation, mechanical ventilation, or surfactant administration during admission. The two cohorts had no significant differences in gestational age, birth weight, or length of stay.
Conclusion(s): Maternal HIV diagnosis, unpartnered status, housing insecurity, and lower educational attainment were associated with maternal psychiatric illness. Very preterm infants born to mothers with mental illness had no significant differences in gestational age, birth parameters, or length of stay. Long-term neurodevelopmental outcome studies are needed, and further research is needed to determine how to better support this higher-risk population.