Neonatology
Session: Neonatal Neurology 3: Clinical
32 - Heart Rate Variability Metrics Correlate with Short-Term Outcomes in Infants with Hypoxic Ischemic Encephalopathy Undergoing Therapeutic Hypothermia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 32
Publication Number: 32.226
Publication Number: 32.226

Desiree Gutmann, MD (she/her/hers)
Pediatric Resident, PGY-3
Lucile Packard Children's Hospital Stanford
Palo Alto, California, United States
Presenting Author(s)
Background: Hypoxic ischemic encephalopathy (HIE) occurs in 1 out of 1000 newborns in the U.S. and despite advances in neonatal care, HIE still has a mortality rate around 15-20%. After the decision to initiate therapeutic hypothermia, there are limited tools that can currently help to predict the extent of brain injury to optimize the newborn’s care and to guide conversations with parents. In previous studies, heart rate variability (HRV) metrics have been shown to correlate with severity of HIE.
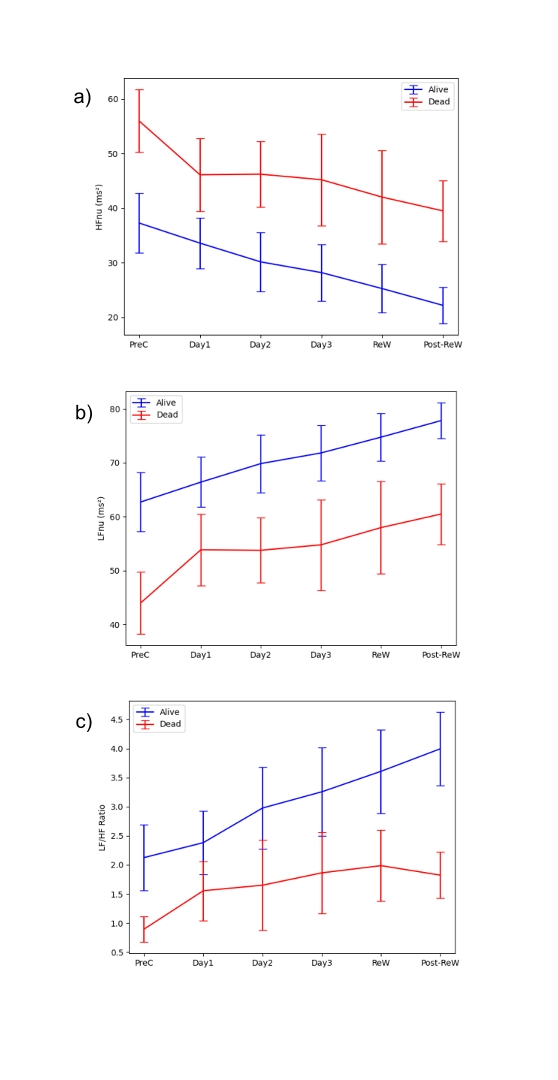
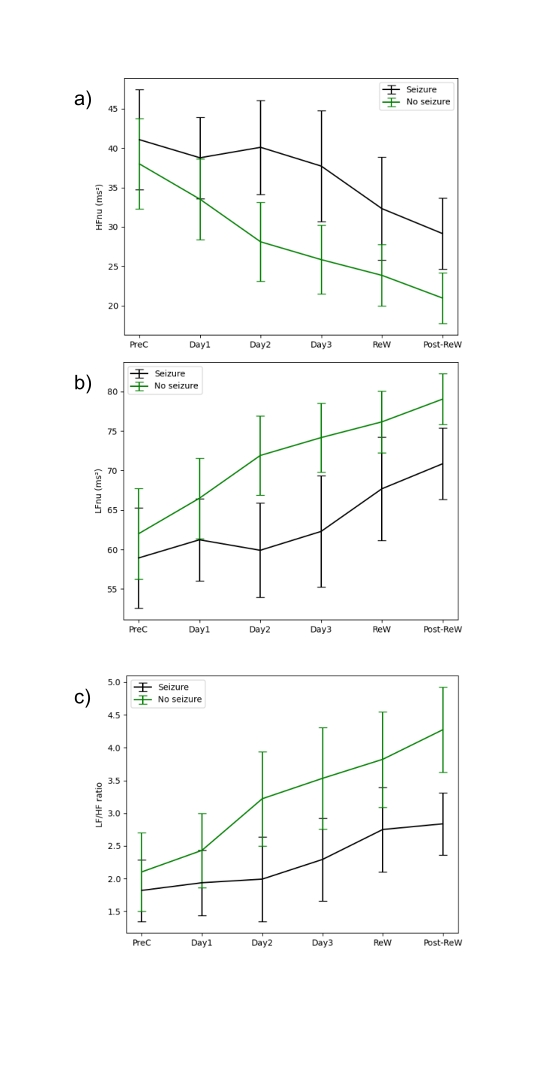
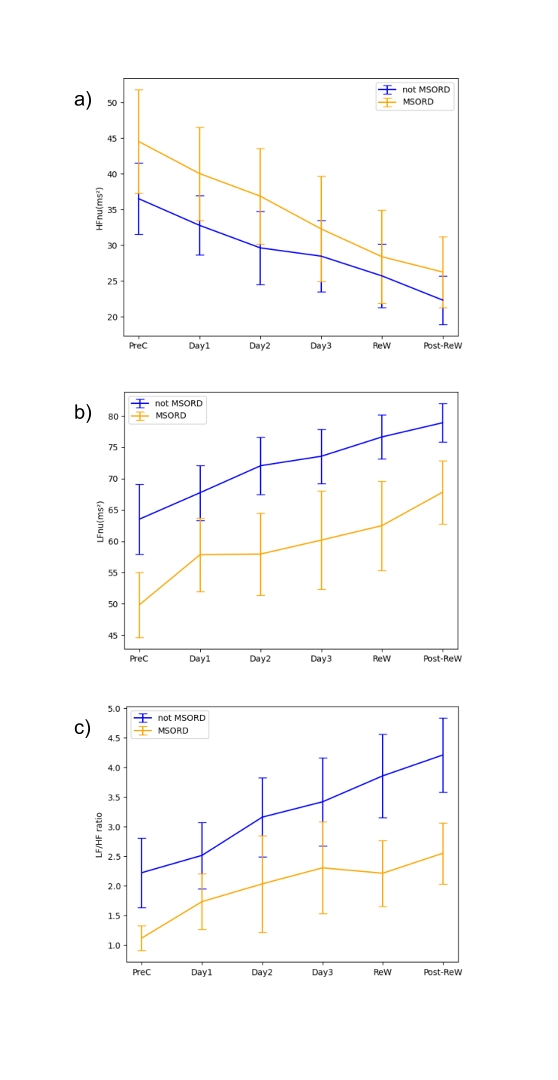
Objective: The aim of the study was to evaluate the temporal changes in HRV metrics in infants with HIE before, during, and after therapeutic hypothermia and correlate those changes with mortality, seizures and the presence of moderate to severe abnormalities on brain magnetic resonance imaging (MRI).
Design/Methods: Single-center retrospective longitudinal observational trial, including patients with HIE, who underwent therapeutic hypothermia in the neonatal intensive care unit between 2016 and 2022. HRV parameters were computed for 6 specific time periods (pre-cooling, cooling day 1, cooling day 2, cooling day 3, rewarming and post-rewarming), over the first 4-7 days of life. Outcome was evaluated in the three categories (1) survival (2) seizures and (3) brain injury on MRI based on Barkovich score. In all categories, HRV metrics of infants with favorable and unfavorable outcomes were compared.
Results: HRV metrics (time domain, frequency domain, and non-linear HRV metrics) were analyzed in 155 patients over a 4–7-day period. This corresponds to 22,000 hours of ECG data (~900 patient-days). For all time periods, normalized low frequency (LFnu) and normalized high frequency (HFnu) power were significantly different and distinguished between favorable and unfavorable outcomes in the categories survival and brain injury on MRI. Similarly, other than the pre-cooling period, normalized LF and HF power were significantly different between patients who had seizures and those that did not.
Conclusion(s): HRV metrics, particularly normalized LF and HF power, offer prognostic insights, starting as early as the first day of cooling. These metrics serve as valuable temporal indicators of mortality, seizures and the presence of moderate to severe brain injury on MRI. Therefore, in the future, HRV metrics might help to predict short-term outcomes in patients with HIE.