Neonatology
Session: Neonatal Fetal Nutrition & Metabolism 4: Nutrition in the NICU
449 - Effects of parenteral nutrition use and age at initiation in neonates treated with therapeutic hypothermia
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 449
Publication Number: 449.1806
Publication Number: 449.1806
Katrina Savioli, MD (she/her/hers)
Staff Neonatologist
Brooke Army Medical Center
San Antonio, Texas, United States
Presenting Author(s)
Background: Recent trials have reported adverse outcomes associated with early initiation of PN in critically ill term neonates. Neonates undergoing therapeutic hypothermia frequently receive parenteral nutrition (PN). In a recent retrospective study in infants receiving therapeutic hypothermia (Gale, Arch Dis Child Fetal Neonatal Ed, 2021), use of PN was associated with increased late onset sepsis and decreased mortality, but the time of initiation of PN in infants receiving therapeutic hypothermia has not been studied.
Objective: To assess morbidity and mortality outcomes of neonates who received therapeutic hypothermia in regards to PN administration and in particular age at initiation of PN.
Design/Methods: This retrospective cohort study included neonates ≥35 weeks gestation admitted to a Mednax-affiliated NICU in 2009-2019. Neonates were matched using propensity scoring to control for demographics and severity of illness. Length of stay was the primary outcome. In infants treated with therapeutic hypothermia, the median age at initiation of PN was 1 day; onset was therefore classified as early if during day of life (DOL) 0, and late if started on DOL 1 or later.
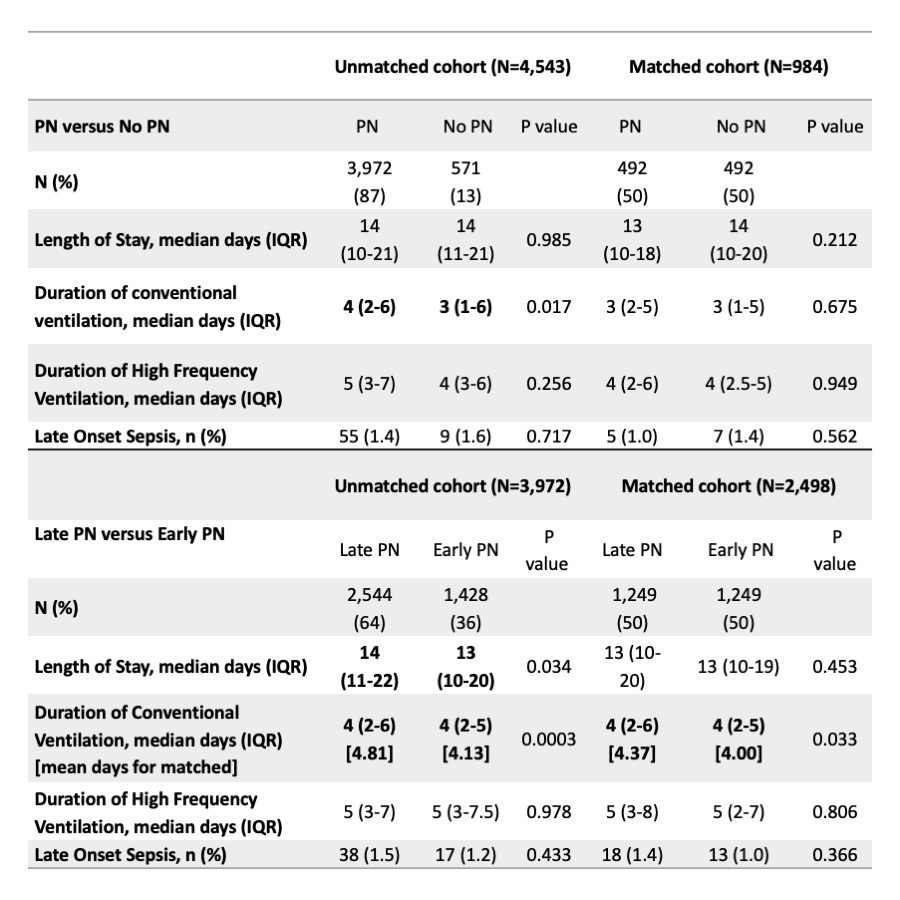
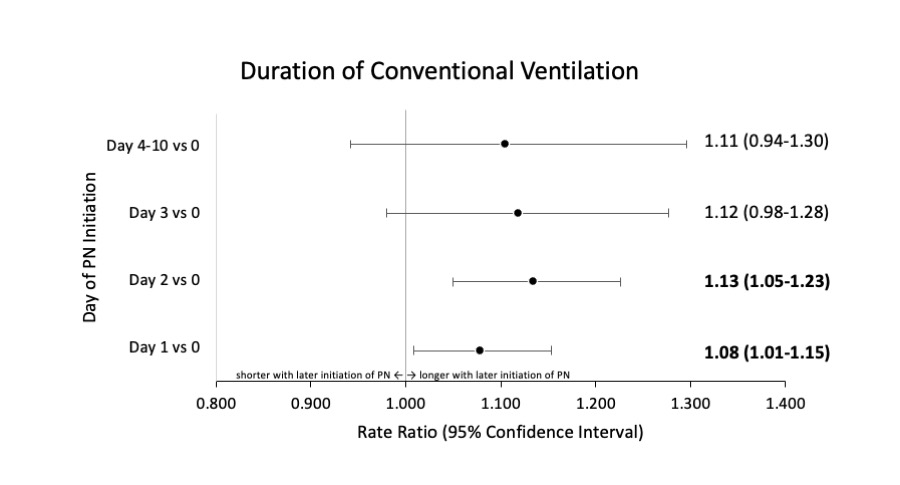
Results: The total cohort included 470,433 neonates, and 3,972 of 4,543 infants (87%) treated with therapeutic hypothermia also received PN. After propensity score matching for PN versus no PN, there were 984 neonates; the 492 matched neonates who received PN had similar length of stay, duration of conventional or high frequency ventilation, and late onset sepsis as the 492 matched neonates who did not receive PN. When comparing late versus early PN (Table), after propensity score matching, 1,249 matched neonates who initiated PN late had increased mean days of conventional ventilation (4.37 versus 4.00; p=0.03) but similar length of stay, duration of high frequency ventilation, and late onset sepsis compared to those who initiated PN early. Compared to early initiation of PN (DOL 0), binomial regression showed increased duration of conventional ventilation when late PN was started on DOL 1 (RR 1.08; 95% CI 1.01-1.15) and DOL 2 (RR 1.13; 95% CI 1.05-1.23) (Figure). There were no differences in mortality outcomes related to PN versus no PN, or early versus late start of PN.
Conclusion(s): Late onset of PN in infants receiving therapeutic hypothermia was associated with a statistically significant increase in respiratory morbidity, but this may not be clinically significant. Receiving PN compared to no PN was not associated with any change in morbidity or mortality.