Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 1
437 - Utilizing a Point-of-Care-Ultrasound Program in a Large Tertiary NICU to Improve Central Line Monitoring and Central Placement
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 437
Publication Number: 437.3264
Publication Number: 437.3264
.jpeg.jpg)
Jack Wren, MD PhD (he/him/his)
Fellow
University of Iowa
Iowa City, Iowa, United States
Presenting Author(s)
Background: Umbilical venous catheters (UVCs) are life-saving devices whose safety and efficacy relies upon their appropriate central positioning. The determination of this positioning has traditionally been X-ray (XR), a modality which has been shown to have poor reliability relative to impractical gold standards such as radiologist-performed ultrasound. In addition to patient safety, UVC efficacy is also maximized by central positioning. This is limited, however, due to the technical limitations of the traditional “blind” insertion approach. Recently, point-of-care ultrasound (POCUS) has been proposed as a solution to both these challenges.
Objective: To investigate the ability of POCUS within a large tertiary NICU to improve (1) UVC tip identification and (2) central placement.
Design/Methods: From July to December 2022; neonatology POCUS (NeoUS) scans were performed twice weekly on neonates with UVCs and the position was interpreted. Lines were classified as appropriate if they were central or low-lying and malpositioned if they were high in the heart or low in the liver. A total of 94 scans were performed and were compared to scheduled line-surveillance XR. For “gold standard” analysis, neonatology-performed US scans were blinded, reviewed, and interpreted by a pediatric radiology fellow (RadUS). Additionally, the POCUS team utilized an US-guided central UVC insertion protocol in cases where the UVC was unable to advance centrally via the traditional approach.
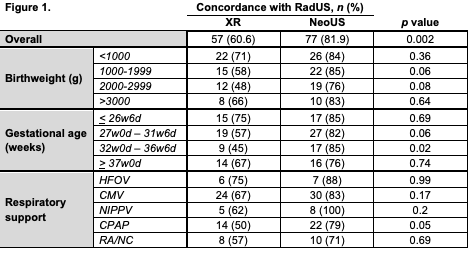
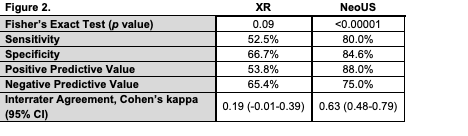
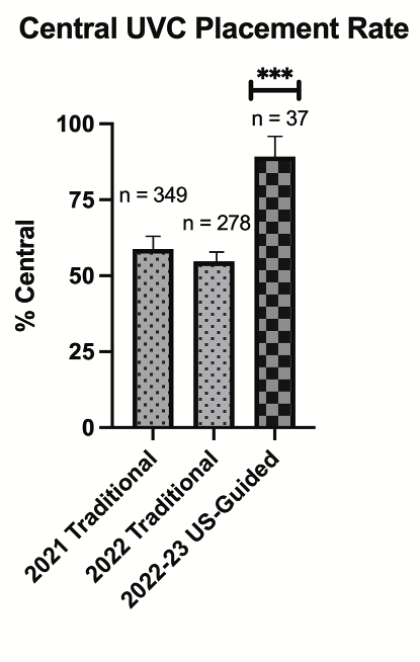
Results: NeoUS was more accurate than XR at identifying UVC location with improved sensitivity (80% vs 52%) and specificity (85% vs 67%). NeoUS exhibited an interrater agreement with RadUS of k=0.634, indicative of substantial agreement (Fig. 1 and 2). Finally, a total of 33 out of 37 infants with UVCs that were initially unable to be positioned centrally (with birthweights ranging from 800g to 4.0 kg) were manipulated to a central position with POCUS (89.2%). This contrasts with our unit’s baseline central UVC rates of 58.7% and 54.7% in 2021 and 2022, respectively (Fig. 3).
Conclusion(s): This study identified that neonatology POCUS was significantly more accurate at identifying UVC location and malposition than the current standard of XR. Further, NeoUS was comparable to a gold standard of radiologist-interpreted US and imminently more available in real-time. Finally, utilizing POCUS for central UVC insertion was both feasible and successful in a general neonatal population including ELBW infants. Taken together, this study demonstrated the use of a POCUS program in a large tertiary referral center to improve UVC surveillance and central insertion.