Neonatology
Session: Neonatal GI Physiology & NEC 1: Necrotizing Enterocolitis
505 - Necrotizing Enterocolitis Prediction using a Novel Heart Rate and Oxygen Saturation Algorithm
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 505
Publication Number: 505.1759
Publication Number: 505.1759
Brynne A. Sullivan, MD, MSCR (she/her/hers)
Assistant Professor
University of Virginia
Charlottesville, Virginia, United States
Presenting Author(s)
Background: Necrotizing enterocolitis (NEC) leads to high morbidity and mortality for very low birth weight (VLBW, < 1500g) infants. Cardiorespiratory changes occur in the early phase of sepsis and NEC. We previously developed a pulse oximetry warning system (POWS) to analyze continuous heart rate (HR) and oxygen saturation (SpO2) data and predict risk of sepsis in the next 24 hours. We hypothesized that POWS would also rise in the preclinical phase of NEC.
Objective: Test the predictive performance of POWS to predict medical and surgical NEC in VLBW infants at four level IV NICUs.
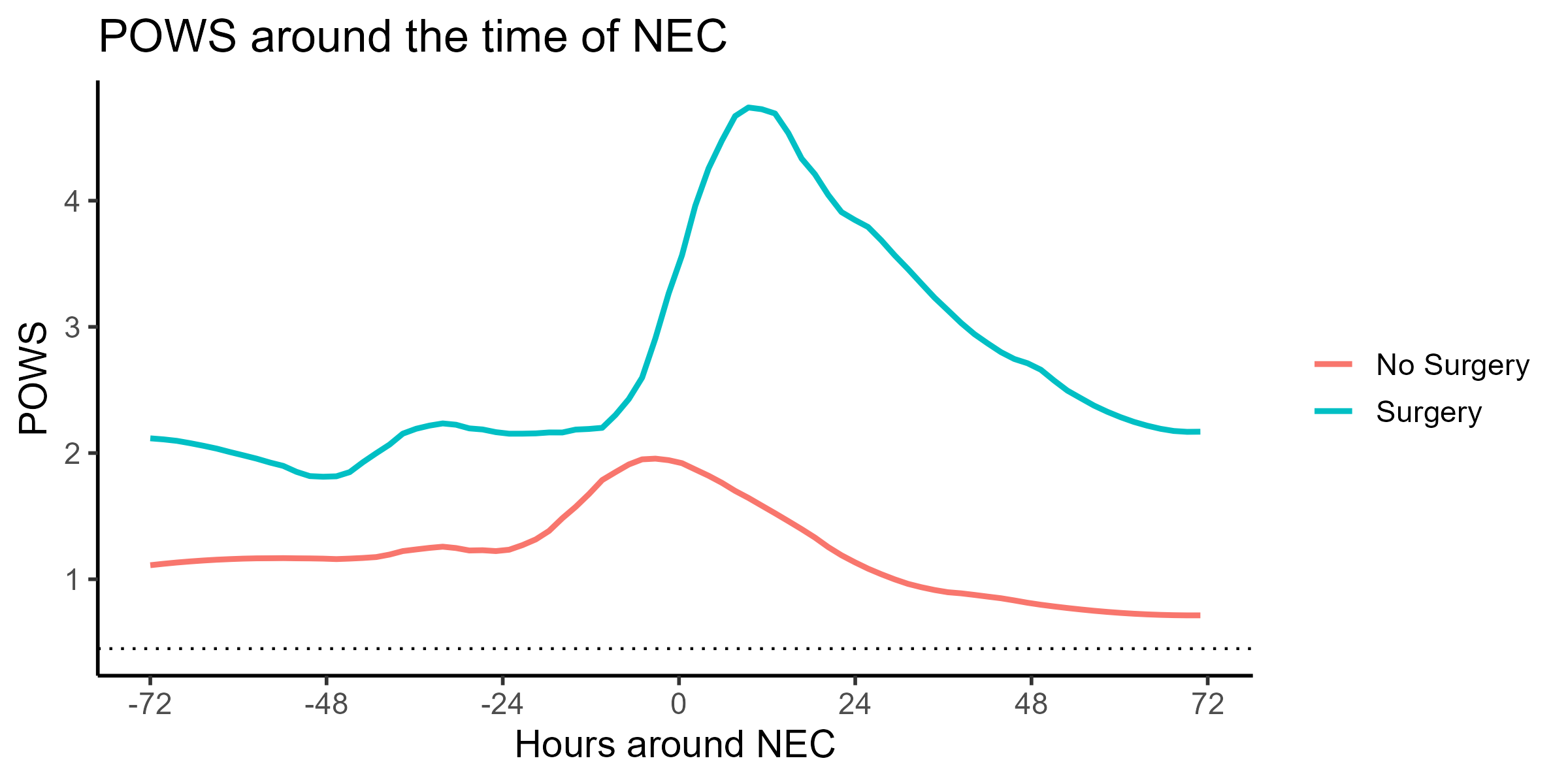
Design/Methods: We calculated POWS for VLBW infants with HR and SpO2 data available and analyzed POWS, demographics, and clinical variables for infants with and without NEC and with surgical compared to medical NEC. Modified Bell's criteria were used to diagnose NEC, and stage II-III cases were included in the analysis. We applied our previously published POWS model to 10-minute windows of HR and SpO2 data to calculate hourly risk predictions from birth to NICU discharge. To examine the dynamic performance near NEC diagnosis, we plotted hourly risk predictions from 72 hours before to 72 hours after surgical and medical NEC diagnosis times. We calculated the area under the receiver operator characteristics curve (AUC) of NEC risk using clinical variables alone and with clinical and POWS risk predictions combined.
Results: We analyzed POWS for 3,050 VLBW infants, of which 142 (5%) were diagnosed with NEC (Table 1). Forty-five (31%) NEC cases required surgery, of which 18 had surgery on the day of diagnosis (12 exploratory laparotomies, 10 drain placements). Infants with NEC had lower birthweight and gestational age than those without (Table 2, p< 0.01). A prediction model using birthweight, gestational age, and small for gestational age status predicted NEC with an AUC of 0.648. POWS predicted any NEC with an AUC of 0.761 and the subset of surgical NEC with an AUC of 0.828. POWS increased from baseline before NEC diagnosis and rose higher and later for infants with surgical compared with medical NEC (Figure 1).
Conclusion(s): In VLBW infants admitted to 4 NICUs, POWS, a cardiorespiratory sepsis risk score, added information to demographic risk factors to predict surgical or medical NEC diagnosis and demonstrated a dynamic rise in risk from baseline near the time of clinical diagnosis.
.png)
.png)
