Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 1: Breastfeeding
464 - Early Formula Supplementation Rates are High and Differ Among Infants by Maternal BMI Class in the PREVAIL Cohort
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 464
Publication Number: 464.1746
Publication Number: 464.1746

Shannon C. Conrey, PhD, MS (she/her/hers)
Postdoctoral Fellow | Instructor
University of Cincinnati College of Medicine
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Formula supplementation early in the perinatal period and maternal obesity are independently associated with reduced breastfeeding duration, but the relationship between these factors is understudied. Baby Friendly Hospital certification requires that only medically indicated formula be given to exclusively breastfed newborns.
Objective: We sought to assess the association between early formula supplementation (EFS), breastfeeding duration, and maternal pre-pregnancy BMI class among mothers with a strong prenatal intention to exclusively breastfeed.
Design/Methods: This analysis includes infants in PREVAIL, a CDC-funded birth cohort in Cincinnati, OH (enrollment 5/2017-8/2018) whose mothers indicated a strong prenatal intention to exclusively breastfeed. Recruitment occurred at two urban birth hospitals; one public, certified Baby Friendly, one private, with a policy to supplement only when medically indicated. Self-reported pre-pregnancy weight and height was used to calculate BMI, categorized as healthy (18.5-24.9), overweight (25-29.9), or obesity (≥30). EFS was defined as self-reported formula use on or before the child’s second day of life. Fisher’s exact test and logistic regression compared proportions and odds, respectively, of infants receiving EFS by maternal BMI class.
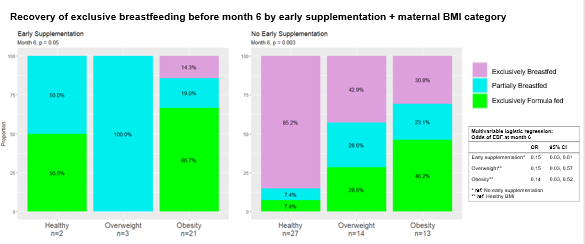
Results: Of 80 mother-infant dyads who participated, 36% (n=29) reported a healthy BMI while obesity prevalence was 43% (n=34). Births were evenly split between hospitals. Approximately 33% (n=26) of newborns received early supplemental formula. However, 7% (n=2) of mothers with a healthy BMI reported EFS compared with 18% (n=3) of mothers with overweight and 61% (n=21) of mothers with obesity (omnibus p< 0.001). Odds of EFS were 29 times higher for mothers with obesity than for those with a healthy BMI when controlling for maternal age (aOR 29.3 (95%CI 6.5-222.5)). Mothers were unlikely to return to exclusive breastfeeding after EFS (aOR 0.15 (95%CI 0.03-0.61), but EFS did not significantly mediate differences in breastfeeding duration by BMI category.
Conclusion(s): Despite strong prenatal exclusive breastfeeding intentions and hospital policies that formula only be given to exclusively breastfed infants when medically indicated, one third of PREVAIL newborns received EFS, with proportions significantly higher in mothers with obesity. Understanding the reasons for EFS as well as the causes of the disparities by maternal BMI may assist in designing interventions to improve rates of exclusive breastfeeding.
.png)
.png)
