Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 4: Congenital Heart Disease
167 - Impact of cardiac cycle phase on ventricular outflow tract diameter measurements for cardiac output calculations in preterm neonates: A clinical validation study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 167
Publication Number: 167.3278
Publication Number: 167.3278
- MG
Macarena Garcia Gozalo (she/her/hers)
FELLOW
Hospital La Paz, Department of Neonatology, Madrid, Spain
Madrid, Madrid, Spain
Presenting Author(s)
Background: Right (RVOTd) and left (LVOTd) ventricular outflow tract diameters are measured routinely in estimation of right (RVO) and left (LVO) ventricular outputs in preterm neonates undergoing targeted neonatal echocardiography (TNE); however, these may vary during systole. The optimal timing to measure RVOTd/LVOTd and validity of calculated RVO/LVO needs investigation. If valid, in patients without any cardiac shunts, calculated RVO should approximate LVO.
Objective: To investigate the variability in RVOTd/LVOTd in relation to different phases of systole and examine the clinical validity of various calculated RVO/LVO paired values.
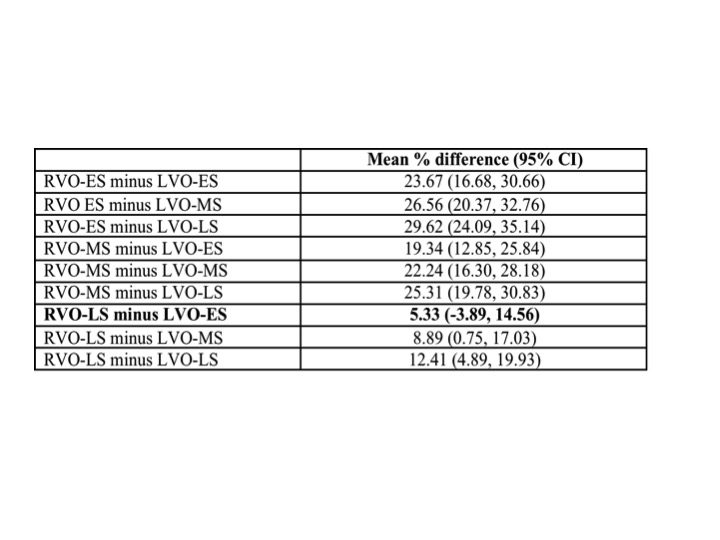
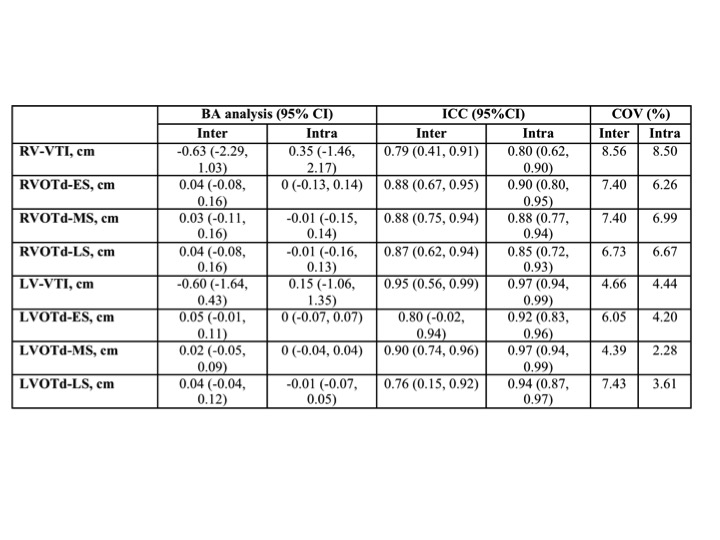
Design/Methods: We did a single-center retrospective study, over 6-year period, including all 56 neonates born < 35 weeks gestation age (GA) who had a TNE with no demonstrable intra- or extra-cardiac shunts. Two independent operators, blinded to other’s analysis, measured RVOTd and LVOTd, respectively at Early- (ES), Mid- (MS), and Late- (LS) systole, to allow calculation of respective RVOs and LVOs using standard formula [(3.14 x radius2 x velocity-time-integral x heart rate)/weight], resulting in 9 RVO/LVO paired combinations for analysis. We describe the overall measurement variability (%), compared values between 3 time points, and calculated mean difference (MD %) and 95% CI for each RVO/LVO pair [(RVO-LVO)/RVO x 100]. A priori, MD ± 15% was considered clinically acceptable. For further clinical validation, in a separate cohort of 25 preterm neonates, >4 weeks old, with exclusive patent foramen ovale (PFO) shunt >2mm, linear correlation between RVO:LVO (Qp:Qs) and PFO diameter was examined for each RVO/LVO pair, using Pearson’s correlation coefficient (r).
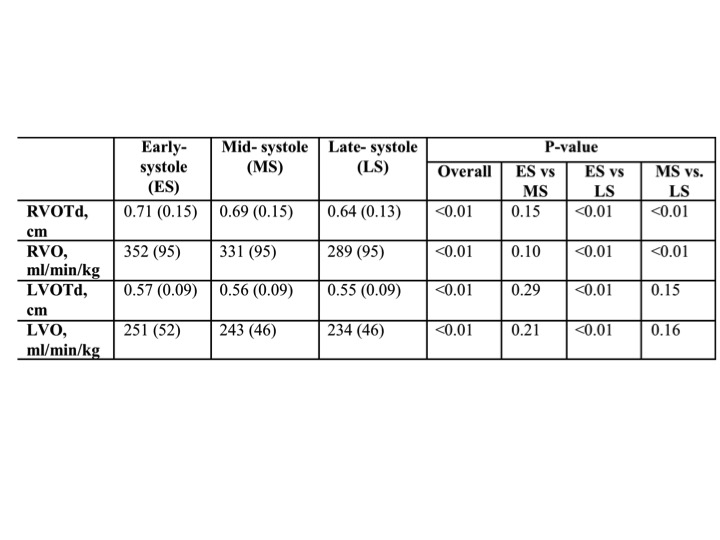
Results: The median (IQR) GA, birth weight and GA at TNE were 25.5 (24.3, 28.1) weeks, 854 (670, 1090) grams, and 34.3 (30.7, 35.71) weeks, respectively. Significant overall variability was seen in indices related to systolic phase at measurement, more for RV than LV [RVOTd vs. LVOTd 13.8% vs. 7.5%, p<.01; RVO vs. LVO 25.3% vs. 14.3%, p<.01]. The stepwise lowering was seen in obtained measurements from ES to MS to LS (Table 1). RVO-LS/LVO-ES pair provided lowest MD with 95%CI < 15% (Table 2). In patients with PFO, among 9 paired combinations, RVO-LS/LVO-ES also had the greatest correlation with PFO diameter (r=0.47, p=0.02). All measured indices demonstrated good inter-observer reliability (Table 3).
Conclusion(s): RVOTd and LVOTd measured in LS and ES, respectively provides clinically valid respective TNE-derived calculations of RVO and LVO in preterm neonates.