Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
354 - Renal Safety QI: Standardizing Medication Reconciliation of Tacrolimus at Discharge
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 354
Publication Number: 354.1690
Publication Number: 354.1690

Bianca E. Saenz, MD (she/her/hers)
Pediatric Nephrology Fellow
Baylor College of Medicine - Texas Childrens Hospital
Houston, Texas, United States
Presenting Author(s)
Background: Accurate dosing of tacrolimus (TAC) is critical to maintain immunosuppression in kidney transplant patients (pts) to prevent rejection and poor graft outcomes. TAC, a narrow therapeutic index medication, should be reconciled with every encounter. Medication prescribing errors at hospital discharge are common and increased with pt medical complexity and provider inexperience. Lack of standardization in medication reconciliation may lead to increased prescribing errors, pt confusion in TAC dose, and poor transplant outcomes.
Objective: Decrease percentage of prescribing errors for kidney transplant pts discharged from the inpatient Renal Service to 0% by October 2023. The process metric will measure adherence of prescribers to the new standardized discharge prescription workflow with a goal of 90%. Additional metric includes improving prescriber confidence of TAC discharge prescription by at least 1 data point on Likert scale.
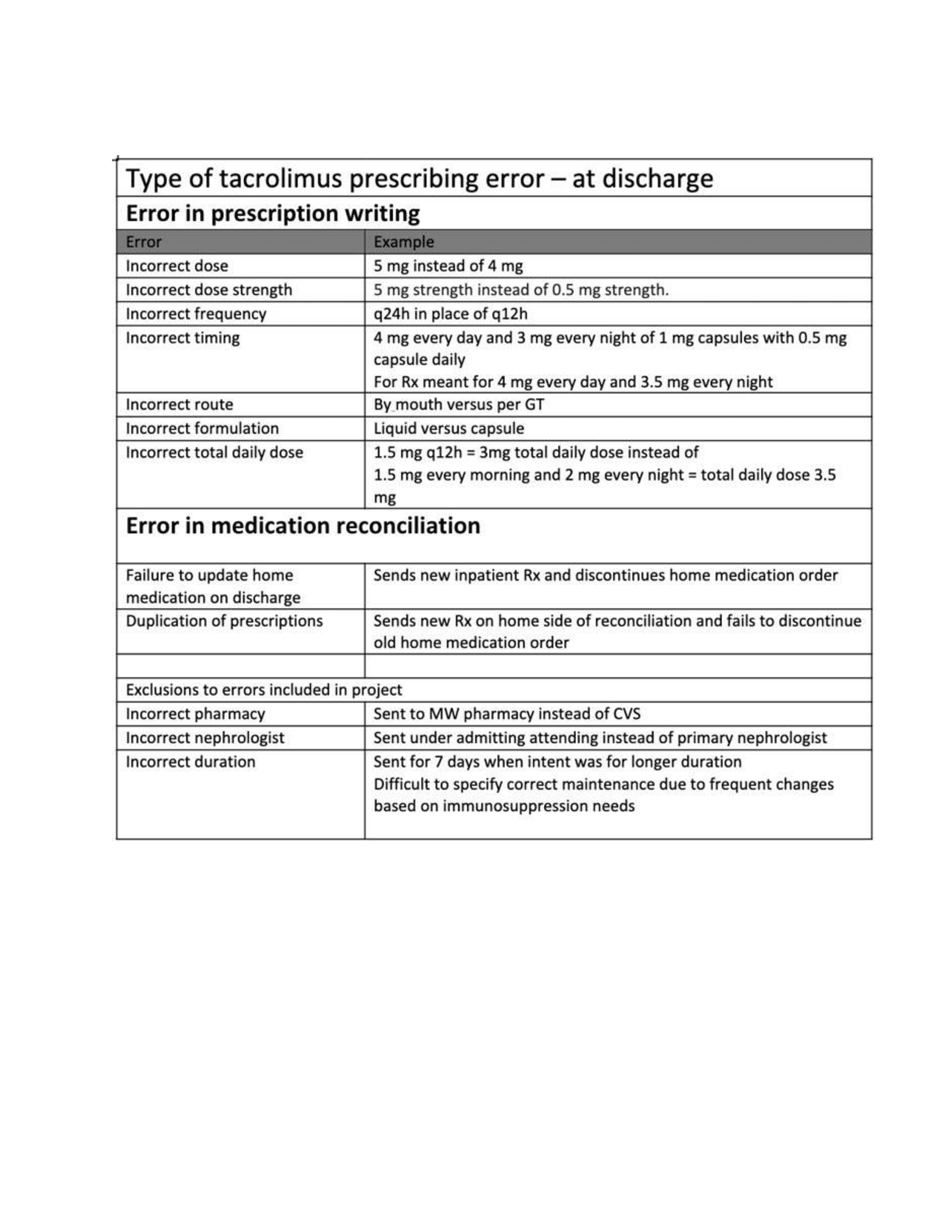
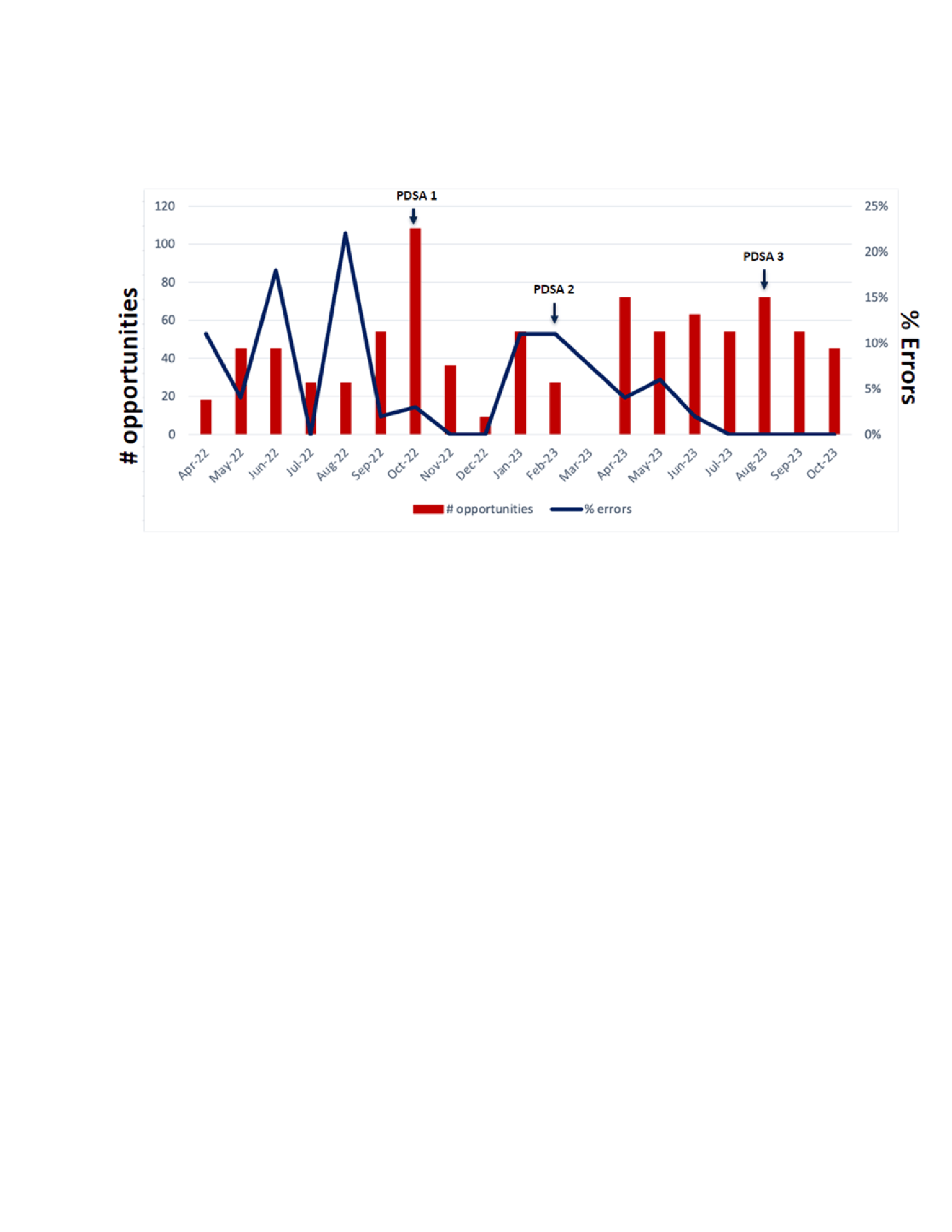
Design/Methods: The prospective quality improvement project was conducted 10/15/2022 – 10/11/2023 at Texas Children’s Hospital. All kidney transplant pts discharged from inpatient Renal Service, excluding admission for transplantation, on TAC whose dose was adjusted during hospitalization were included. Fishbone diagram identified prescriber inexperience and variation in medication reconciliation as factors leading to prescribing errors. Each encounter was evaluated for nine potential prescribing errors. PDSA (Plan Do Study Act) cycles included standardization of TAC reconciliation, education for trainees, and post-discharge smart phrase documentation with transplant coordinators. Subsequent cycles surveyed barriers to adherence and implementing senior resident role in reviewing discharge TAC prescriptions.
Results: TAC dose was adjusted in 72 pt encounters. There were 648 opportunities for prescription error. Baseline data had 8.8% (19/216) errors which improved to 2.93% (19/648) over the study period. Prescription errors were 0% by end of last PDSA cycle. 81% of prescribers adhered to standardized process and confidence in TAC reconciliation increased following education. All pts had a post discharge follow up with transplant coordinator, 4.2% were noted to be taking incorrect dose.
Conclusion(s): Accurate medication reconciliation of TAC is critical in ensuring correct dose. Although prescriber knowledge and confidence in TAC reconciliation improved, adherence to standardized process was not at goal. Future PDSA cycles will focus on adherence to new workflow and reviewing rates of rejection amongst pts involved in study period.
.png)