Emergency Medicine
Session: Emergency Medicine 12: Potpourri
425 - Procedural Exposure and Competency in Pediatric Emergency Medicine Fellowships: How Are We Tracking Expected Procedures and What Are We Doing When Direct Patient Care Is Not Enough?
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 425
Publication Number: 425.3340
Publication Number: 425.3340

Madeline R. Field, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Medical College of Wisconsin
Wauwatosa, Wisconsin, United States
Presenting Author(s)
Background: The ACGME provides a list of essential procedural skills for PEM fellow graduates. But limited exposure to some procedures may impact proficiency and confidence.
Objective: To examine if and how PEM fellowship programs track fellow-performed procedures, to determine whether programs have a predesignated number of procedures required to achieve “competence,” to assess if fellows are reaching these thresholds in clinical care alone, and to understand how programs are providing exposure to procedures unable to be mastered by clinical exposure alone.
Design/Methods: Program directors from the 85 accredited PEM Fellowship programs in the United States were surveyed. The survey contained demographic questions on program/hospital type, if and which procedures were tracked, the “threshold for competence” number for each procedure, and how programs are providing educational experiences for procedures not achieved through direct clinical alone.
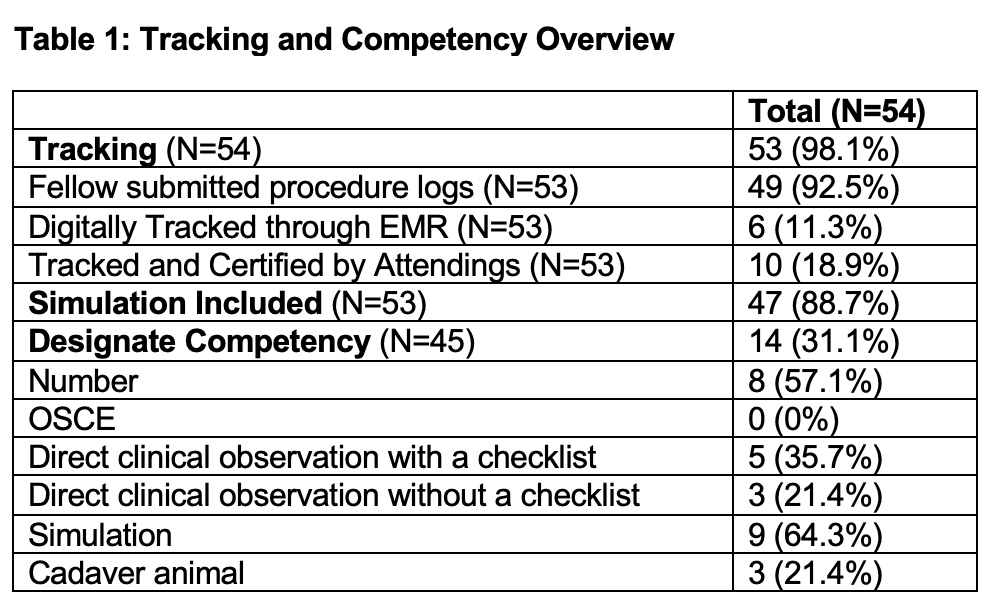
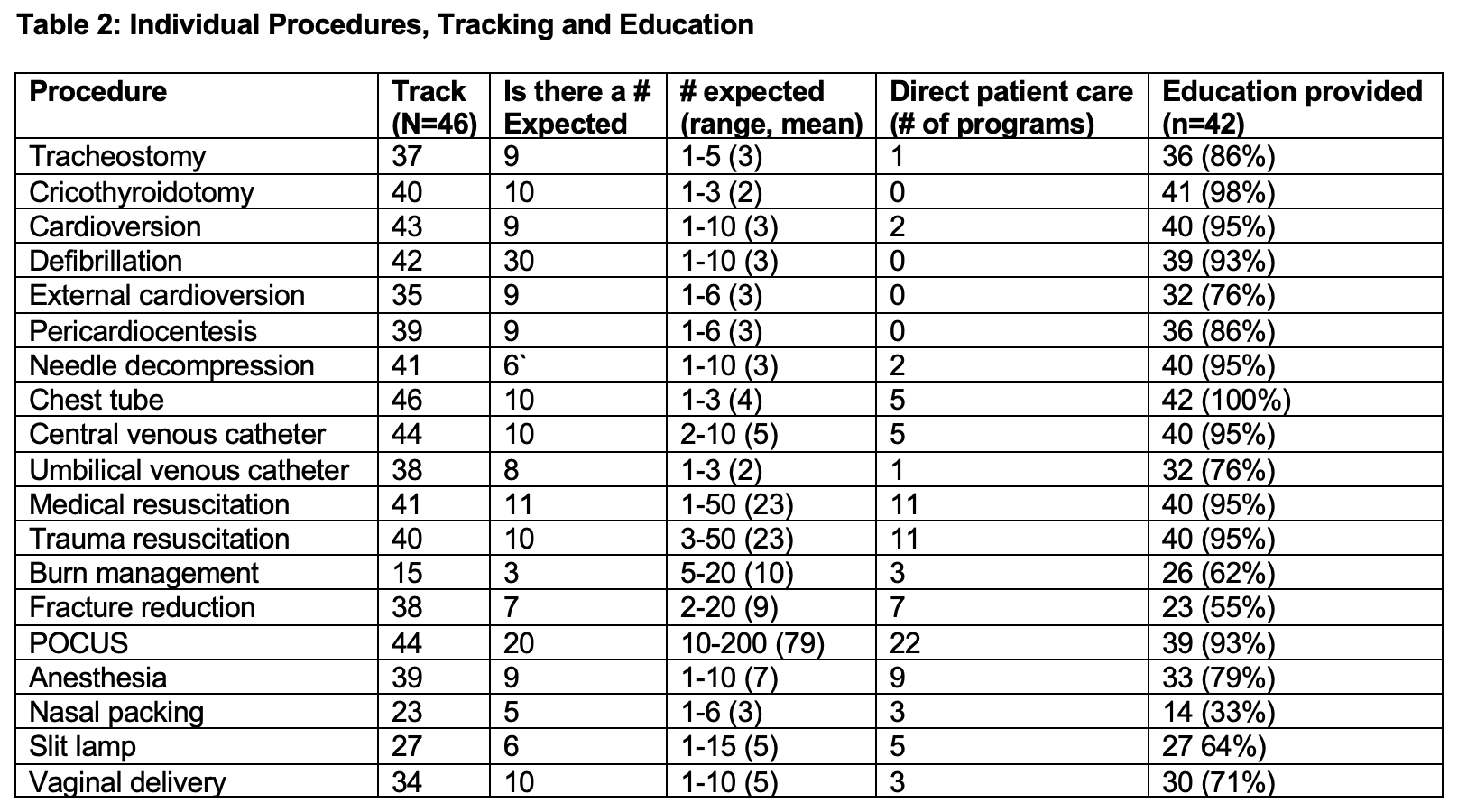
Results: 54 (64%) of program directors responded with 40 (47%) completing the survey. Most were from level 1 (32, 80%) trauma centers, with a minority working in level 2 (5, 12.5%) and level 3 (3, 7.5%) trauma centers. A majority, 20 (50%) had patient volumes >75,000, with less respondents working in hospitals with smaller annual volumes 10 (25%) 50-74,999, 10 (25%) 20-49,000. Nearly all (98%) reported tracking fellow performed procedures, with the majority 49 (91%) tracking via fellow submitted procedure logs. 32 (59.3%) of programs reported designating achievement of procedural competency, with preset numerical thresholds and simulation being the most common methods of achievement (Table 1). Four of the procedures had zero programs achieving the desired numbers through direct patient care alone with all procedures having < 50% of programs achieving them through direct patient care (Table 2). The designated number to achieve competency in each procedure varied greatly and the number of programs providing additional education for each individual procedure is listed in Table 2.
Conclusion(s): Programs are tracking their fellow’s procedures, but direct clinical care experiences are not enough to ensure competence. There are many strategies being used to enhance procedural training but there is no consistent educational standard amongst programs. Procedures that cannot be acquired solely through direct patient care may require a differentiation between exposure and competency. This information may lead to the modification of ACGME requirements and should emphasize the importance of collaboration between programs to share best practices in procedural education.