Neonatology
Session: Neonatal General 9: Outcomes, Genetics. Ethics
386 - Predictive Factors for Timely Achievement of Oral Feeds in Newborns ≤1250 Grams
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 386
Publication Number: 386.2718
Publication Number: 386.2718
- PP
Prabhu S. Parimi, MD, MBA (he/him/his)
Division Chief, Neonatology
MetroHealth Medical Center
Cleveland, Ohio, United States
Presenting Author(s)
Background: Preterm babies commonly have aerodigestive difficulties secondary to the systematic immature development of their tissues and organs. The resulting difficulty in breathing and swallowing negatively affects their subsequent food intake, growth, and development. This leads to longer hospital stays and costs and potentially worsens outcomes for the babies later in life (Kamity et al. 2021). The relationship between early referral to Speech language pathologists (SLP) and full oral feeds achievement is not as well studied as it is for certain other neonatal morbidities, and so is of particular interest to this study.
Objective: The purpose of this study is to determine referral patterns of babies to SLP and to determine predictive factors that influence feeding progression in low-birth-weight infants. We hypothesize that birth weight, gestational age and respiratory and digestive comorbidities play a role in timely achievement of oral feeds.
Design/Methods: Design: Retrospective Chart Review
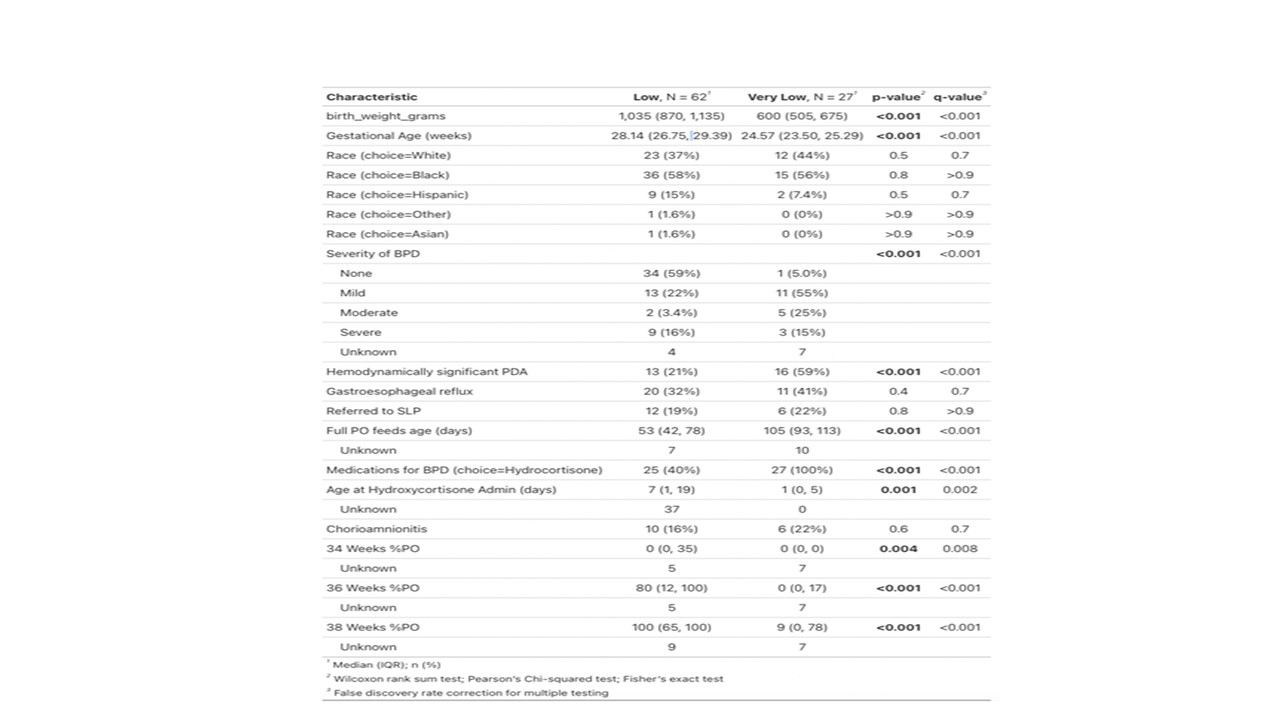
Preterm infants with a birth weight ≤1250 g (n=89) born between Jan 21-December 2022 were selected. A data abstraction form was designed in Redcap. Demographic and clinical data, severity of BPD, presence or absence of HsPDA, time to full PO feeds, and percent of PO feeds at 34 weeks, 36 weeks and 38 weeks was collected (Table 1). The characteristics of the entire group and chosen subgroups were ascertained and compared. A regression model was developed to determine the independent predictive power of each variable on feeding outcomes. The analysis was performed in R.
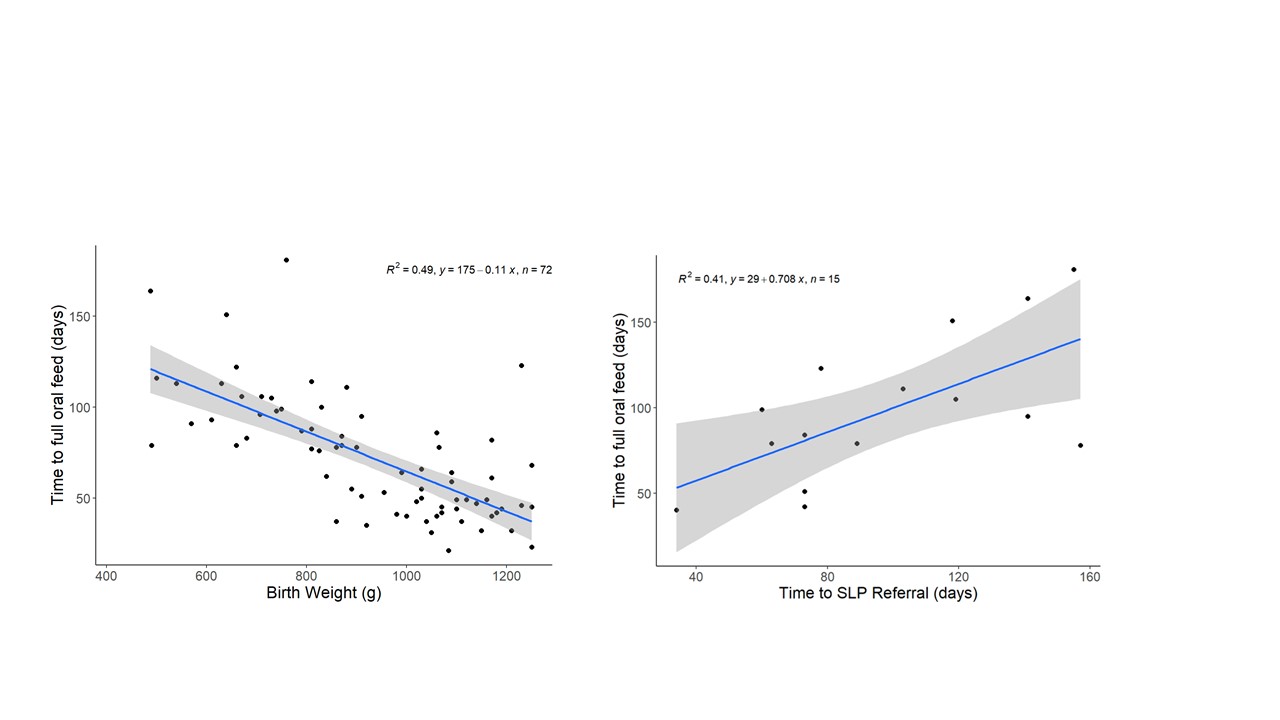
Results: Percent of per oral feeds in preterm infants < 750g and < 28 weeks gestational age were significantly lower at 34, 36 and 38 weeks of corrected age (p <.001). The mean age of full PO feeds was 105 days. Despite cue-based feeding guideline, the lower gestational age and associated clinical morbidities contributed to delayed achievement of full PO feeds. 20% of preterm infants were referred to SLP (Table 1). Birth weight is inversely related to full PO feeds and delayed SLP referral led to delayed achievement of full PO feeds (Figure 1).
Conclusion(s): The infants being referred to SLP in this NICU are those who take longer to feed, have more comorbidities, and are more likely to be white. Among those who are referred, earlier referral predicts sooner achievement of full oral feeds. These data are of clinical significance and suggest that criteria to refer patients to SLP could result in improved feeding progression and decrease in length of NICU stay.