Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 9
333 - Neighborhood Characteristics and Acute Care Utilization in Childhood Nephrotic Syndrome
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 333
Publication Number: 333.1940
Publication Number: 333.1940
Emily Frierson, MD (she/her/hers)
Pediatric Nephrology Fellow
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: Childhood nephrotic syndrome (NS), most commonly due to minimal change disease (MCD), has wide variation in severity, chronicity, and long-term outcomes. While there is active research into the genetic underpinnings of these differences, little is known about the influence of neighborhood-level factors on patient outcomes.
Objective: This study evaluates the association between neighborhood disadvantage and acute care utilization among children with children with MCD. It was hypothesized that greater neighborhood disadvantage is associated with increased acute care utilization.
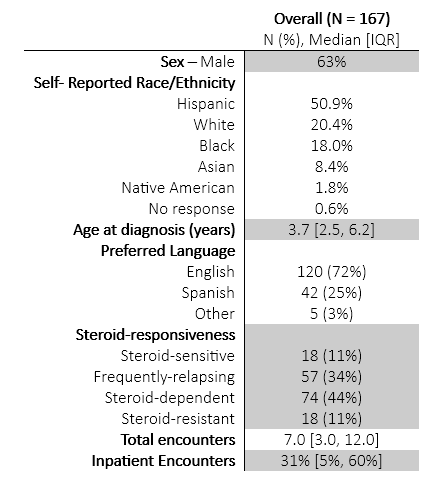
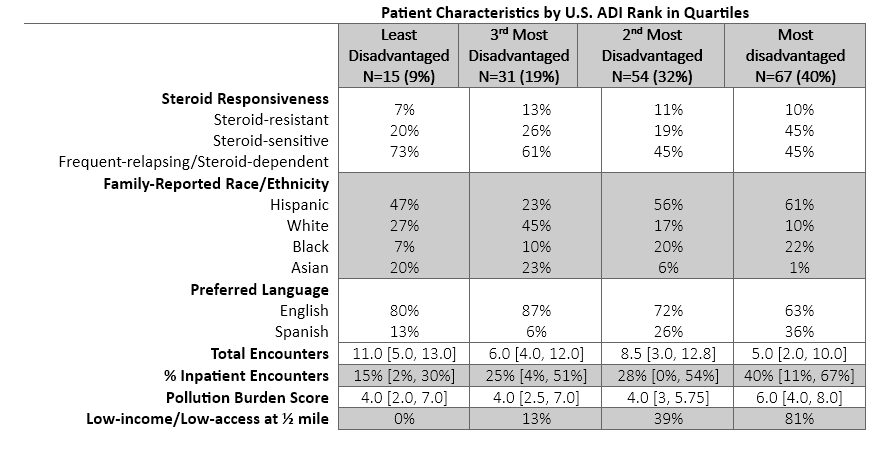
Design/Methods: This is a single-center, retrospective study of children with MCD diagnosed between 2011 and 2020. Collected data included demographics, steroid response, and acute care encounters for NS. Standard definitions were used to define steroid-dependent, frequent-relapsing and steroid-resistant NS. Number of encounters that required a medical intervention for acute NS relapse and/or associated fluid-overload was used as a proxy for acute care utilization. Area Deprivation Index (ADI) was used to assess socioeconomic disadvantage using patient address at diagnosis. Access to healthy food and burden of environmental pollution were additional measures of neighborhood disadvantage studied using data from the USDA Food Access Research Atlas and the Environmental Protection Agency, respectively.
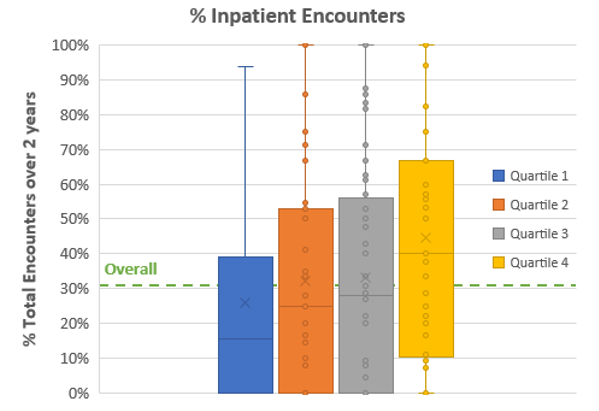
Results: 217 patients were reviewed for study inclusion. We excluded patients if the first episode occurred outside of Texas; they had less than two-years of follow-up, or were seen for second opinion visit (n=50). A total of 167 patients were included. 40% (n=67) of patients live in most disadvantaged neighborhoods, where more homes are considered low-income with low-access to health food, and burden of pollution highest. Patients had proportionally more hospital/ER encounters as neighborhood disadvantaged increased. A multivariate linear regression with ADI as the predictor of number of encounters showed a statistically significant association between ADI and number of encounters (β = -.16; p <.02), controlling for race/ethnicity, language, distance to care and steroid responsiveness.
Conclusion(s): Our findings suggest that neighborhood disadvantage is associated with encounters for relapse and fluid-overload among children with MCD. ADI may be used to inform providers which patients are at higher risk for frequent acute care utilization. Further research is needed to evaluate the impact of place and health to inform equitable allocation of resources towards children that live in disadvantaged neighborhoods.