Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 2
496 - Validation of a risk-prediction model for pediatric post-discharge mortality at two hospitals in Rwanda
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 496
Publication Number: 496.311
Publication Number: 496.311
- AH
Anneka Hooft, MD, MPH (she/her/hers)
Assistant Clinical Professor
University of California, San Francisco, School of Medicine
Oakland, California, United States
Presenting Author(s)
Background: Mortality following hospital discharge remains a significant threat to child health, particularly in resource-limited settings. In Uganda, the Smart Discharges risk-prediction models have demonstrated success in their ability to predict those at highest risk of death after discharge and use this to guide a risk-based approach to post-discharge care in children admitted with suspected sepsis. These prediction models have not yet been validated outside of Uganda.
Objective: This study aims to externally validate these models within the Rwandan context.
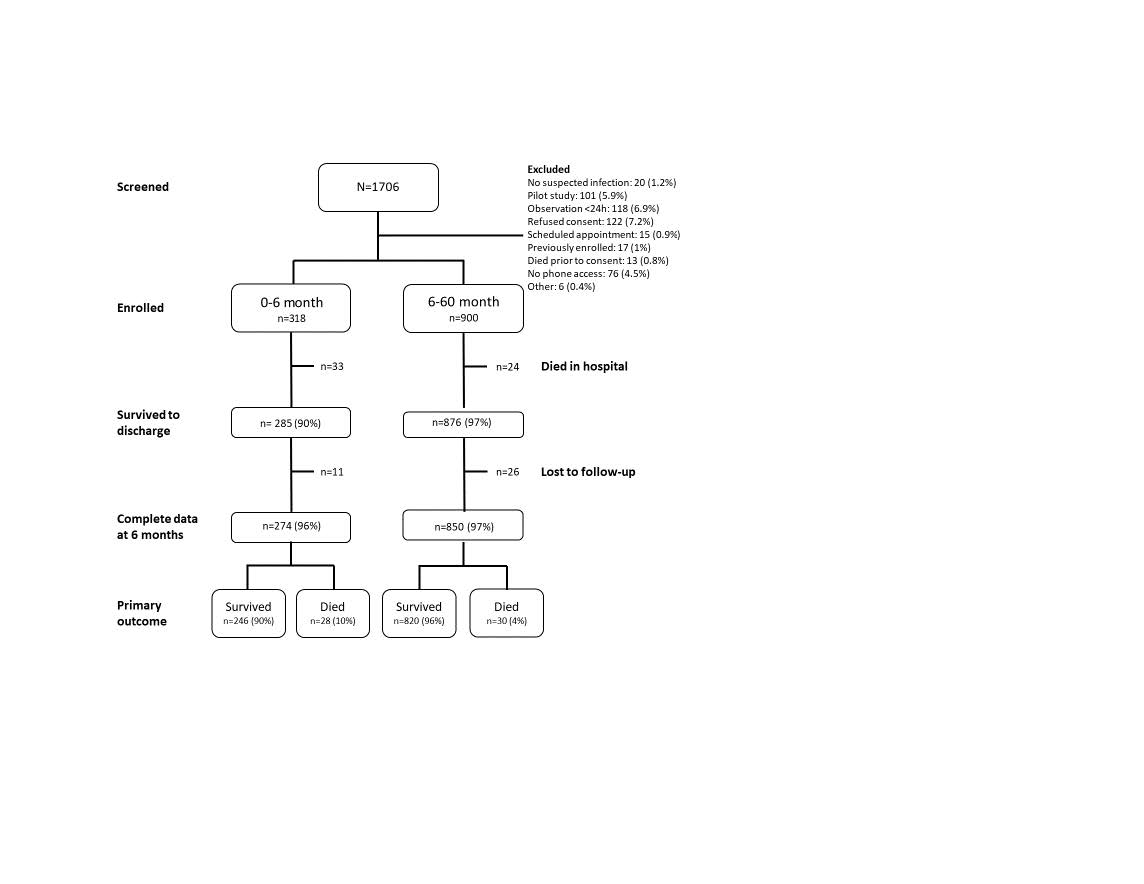
Design/Methods: We prospectively recruited children 0 days-60 months admitted with suspected sepsis at two hospitals in Rwanda: Ruhengeri Referral Hospital in Musanze (rural) and University Hospital of Kigali in Kigali (urban). Enrollment occurred between May 2022 to February 2023. All children were followed up to determine vital status as 6 months post-discharge. Five previously reported and derived models from the Smart Discharges Uganda cohort were validated in this cohort: two models for children 0-6 months, and three for children 6-60 months. Within each age cohort, some models focused on clinical variables alone while others included a mixture of clinical and social variables. Validation performance was evaluated by calculating the area under the receiver-operator curve (AUROC). Model calibration was visualized using calibration plots.
Results: We enrolled 1218 children (n=413, Kigali; n=805, Ruhengeri). Of the 1161 live dischargees, 1123 completed follow-up (96.7%). The overall rate of post-discharge mortality was 4.8% (n=58). All five prediction models tested achieved an AUROC greater than 0.7 (range 0.706 - 0.738). Low event rates resulted in moderately wide confidence intervals. Model degradation, as determined by the percent reduction in AUC between the original model and the derived model, ranged from 1.1% to 7.7%. Calibration plots showed good calibration for all models at predicted probabilities below 10%. There were too few outcomes to assess calibration among those at higher levels of predicted risk.
Conclusion(s): We externally validated five risk-based prediction models for post-discharge mortality of children admitted for infection in two hospitals in Rwanda. Discrimination was good, despite low outcome rates. Further work to assess calibration among higher risk groups in Rwanda is required to ensure models are broadly generalizable to all children with suspected sepsis in Rwanda and in similar, resource-limited settings.
.jpg)
