Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
374 - Implementation of a Validated Developmental Screening Tool in an Ambulatory Care Clinic: Survey of Wellbeing in Children (SWYC)
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 374
Publication Number: 374.2025
Publication Number: 374.2025
- YM
Yusuke Matsuura, MD (he/him/his)
Resident
Mount Sinai Hospital
New York, New York, United States
Presenting Author(s)
Background: Developmental disabilities are common and are underdiagnosed in primary care. The AAP recommends the use of a validated developmental screening tool at 9,18, and 30-month well visits to help detect delays and maximize the impact of early intervention services. To address the lack of standardization of developmental screening in our resident clinic, we launched a QI project to implement a validated questionnaire, the Survey of Wellbeing in Young Children (SWYC). Our global aim is to promptly identify development delays and improve long-term outcomes for our patients.
Objective: By June 2024, we aim to use the SWYC at 50% of 9–30-month-old well child visits, with equal utilization between English and non-English speaking patients.
Design/Methods: Stakeholder input informed the creation of a process map and helped identify potential failures and key drivers. Our primary outcome measure is the percentage of eligible patients with a completed SWYC documented in the electronic medical record (EMR). Our process measure is the percentage of eligible patients with a completed paper SWYC on arrival. SWYC implementation began with the introduction into the EMR on 11/14/2022. Data collection continued through multiple PDSA cycles.
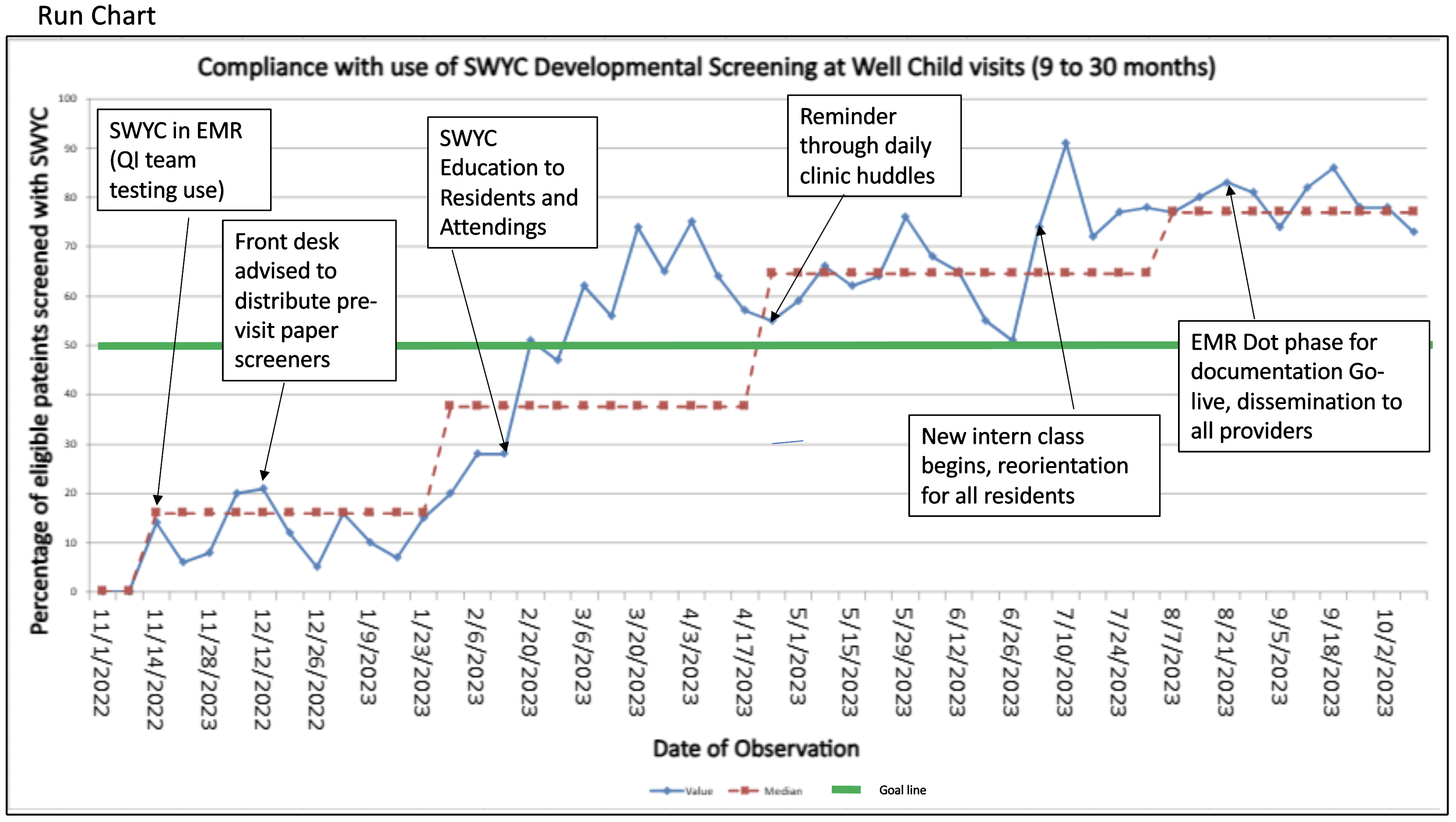
Results: Prior to implementation, baseline SWYC screening rate was 0%. Incremental success with each PDSA cycle allowed for multiple recalculations of the median (16 to 37.5 to 64.5 to 77%). Compliance surpassed our goal of 50% within 5 months into the intervention period. Our successful interventions included education of providers via didactics, emails, clinic huddles, and EMR changes, including an Epic smart phrase for documentation. (Figure: Run Chart). Our process measure tracked fewer than 5 paper screeners completed per week, largely due to workflow challenges around distribution of age-based paper questionnaires.
Conclusion(s): This QI initiative demonstrated rapid uptake of a standardized developmental screening tool. Success can be attributed to individual behavior change resulting from numerous educational interventions as well as culture change with incoming residents. Distribution of pre-visit paper questionnaires was not a viable process in our clinic, but we plan to introduce a pre-visit SWYC via patient portal to decrease provider burden and augment screening. Additional data analysis will compare rates for English and Non-English-speaking patients. Given concerns that utilization of patient facing questionnaires could impact resident learning of developmental milestones, we plan to track trends on In-Training scores within the development domain as a balancing measure.