Neonatology
Session: Neonatal/Infant Resuscitation 3
295 - Impact of Delivery Room Specific Critical Congenital Heart Disease Learning Modules on Management of Congenital Heart Block - A Multi-centered Educational Intervention and Simulation Study
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 295
Publication Number: 295.3005
Publication Number: 295.3005

Danielle Reed, MD (she/her/hers)
Attending Neonatologist
Children’s Mercy-Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: Neonates with critical congenital heart disease (CCHD) require disease-specific delivery room (DR) management. For example, a neonate with complete congenital heart block (CHB) in the DR requires early hemodynamic assessments and prioritizes chronotropy over chest compressions (CPR) and bolus epinephrine for hemodynamic instability. Such alterations are not routinely discussed in traditional DR resuscitation training, leaving an educational gap
Objective: We aim to evaluate CCHD DR management eLearning modules through acceptance surveys, pre/post knowledge tests, and simulation performance.
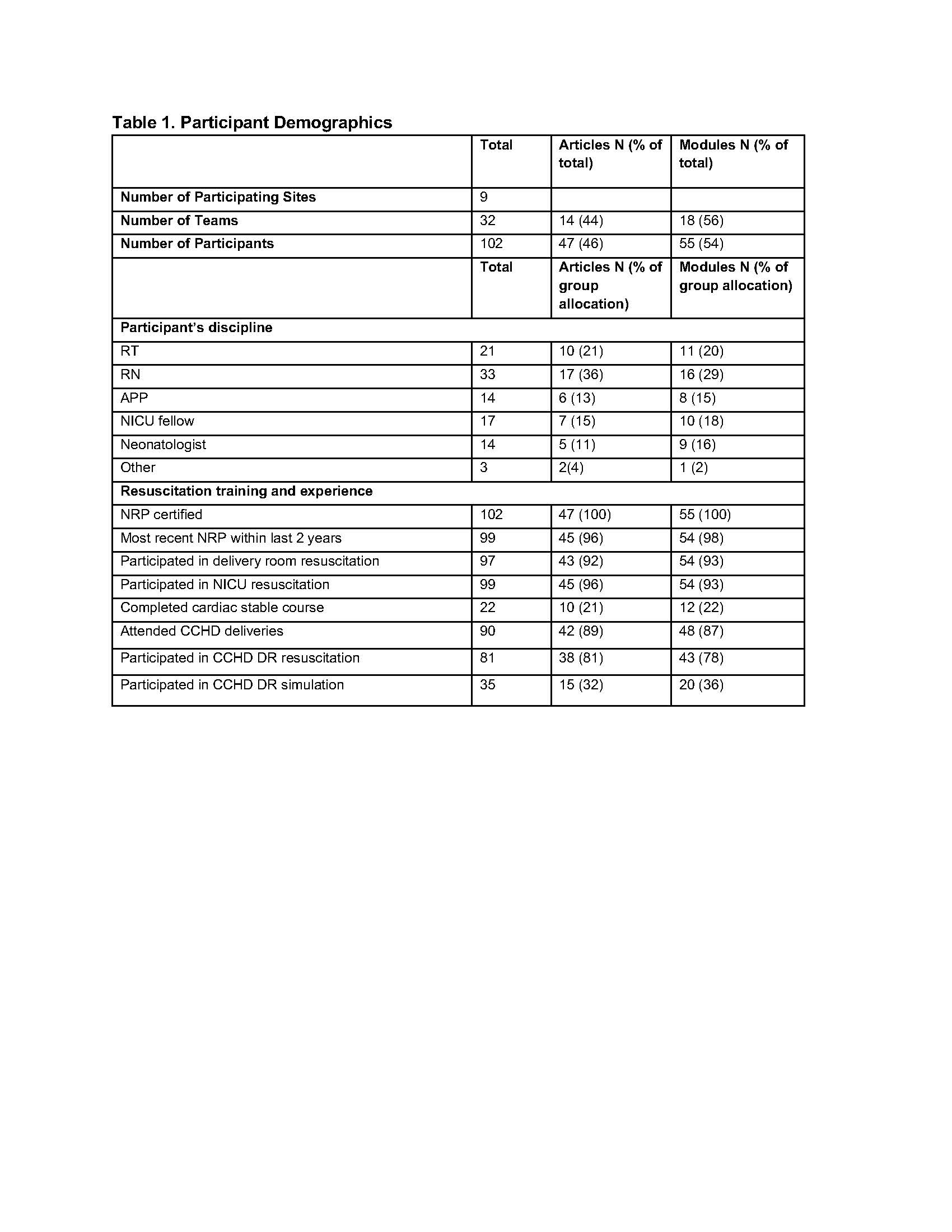
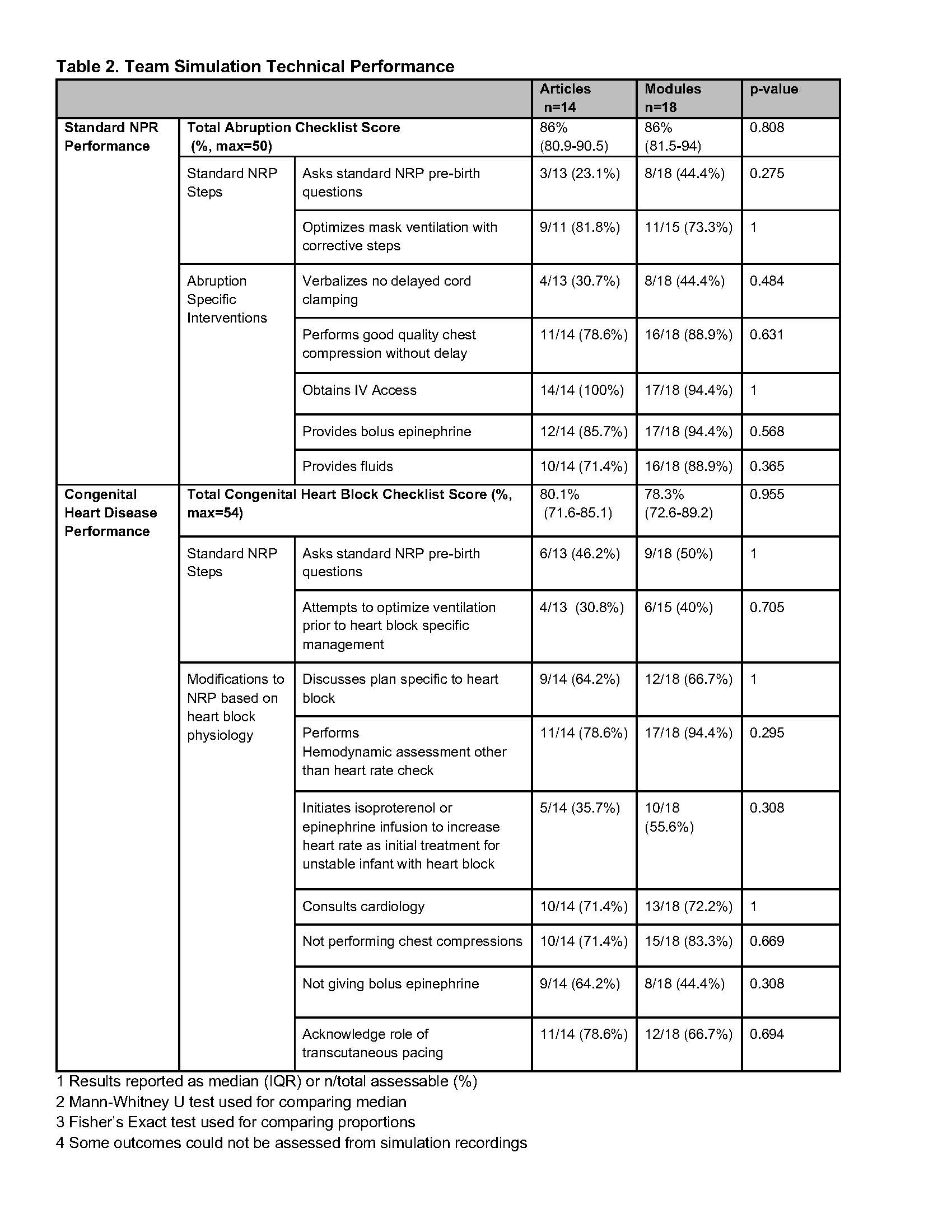
Design/Methods: This was a multi-centered educational intervention and simulation study. As a part of the DeveLopment of EducationAl Modules for Resuscitation of Neonates in the Delivery Room with Congenital Heart Disease (LEARN-CHD) study, teams of neonatal healthcare providers (HCPs) were randomized to receive CCHD journal articles (control) or eLearning modules (intervention). Module group HCP’s rated module acceptability. All HCPs submitted pre and post intervention knowledge tests, then participated in team simulations to assess technical performance on baseline neonatal resuscitation (abruption) and specific CHD scenarios. The CHB scenario was designed to avoid CPR and epinephrine boluses if chronotropy treatment was initiated. Simulations were video-recorded and scored by raters blinded to allocation using scenario-specific performance checklists. The performance of critical interventions was compared between groups.
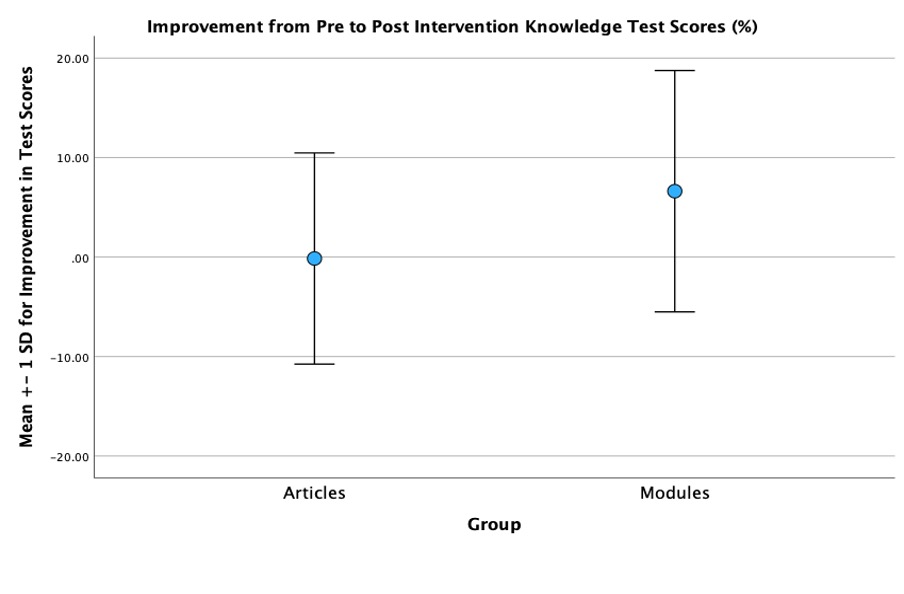
Results: 32 teams from 9 centers participated (n=102, Table 1). 87% of Module group HCPs felt that the modules were more effective than traditional educational methods.(Figure 1A) Modules group HCPs demonstrated improvement in knowledge test scores after the intervention (mean change 6.6+/-12.1%), compared with no improvement (-0.1+/-10.6%) in the Articles group (p=0.008) (Figure 1B) In simulations, there was no difference between groups in teams technical performance checklist scores in either abruption or CHB scenarios. A higher proportion of Module teams assessed hemodynamics, avoided CPR for bradycardia, and prioritized critical CHB-specific treatments. (Table 2) Both groups had significant rates of bolus epinephrine use in unstable CHB.
Conclusion(s): Delivery room specific CCHD learning modules were well-accepted by HCPs and resulted in improved post-intervention knowledge scores. Simulation performance in CHB management was similar. Ongoing education development for DR management for CCHD is required.