Neonatology
Session: Neonatal Neurology 3: Clinical
41 - Feeding Problems in Neonates with Hypoxic Ischemic Encephalopathy Treated with Therapeutic Hypothermia and Association with Brain MRI and EEG Abnormalities
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 41
Publication Number: 41.538
Publication Number: 41.538
- CA
Ceyda Acun, MD (she/her/hers)
Associate professor
Cleveland Clinic Children's Hospital
Cleveland Clinic Children's Hospital
Cleveland, Ohio, United States
Presenting Author(s)
Background: Hypoxic Ischemic encephalopathy (HIE) is a major cause of morbidity and mortality in neonates. Early brain injury is known to have a deleterious impact on oral motor functions, which may lead to feeding and speech problems.
Objective: To evaluate the prevalence of swallowing impairment and its association with brain magnetic resonance imaging (MRI) and electroencephalogram (EEG) abnormalities in neonates with HIE and treated with therapeutic hypothermia (TH).
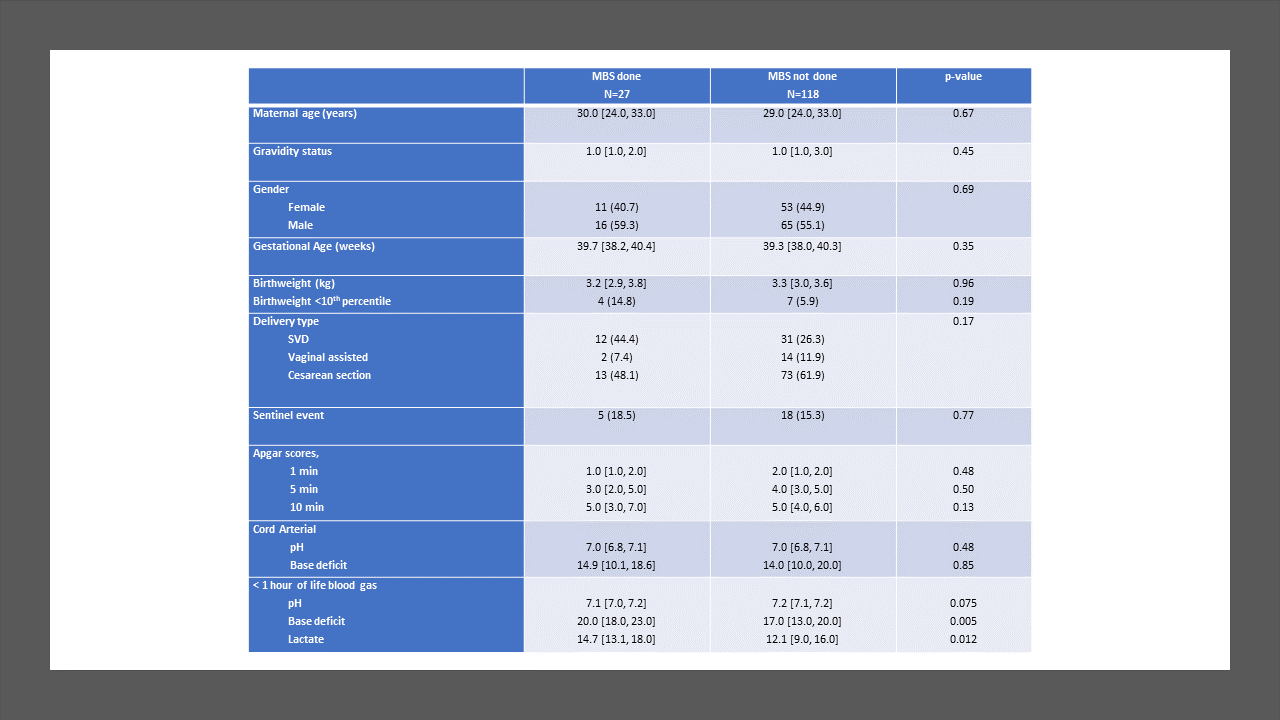
Design/Methods: This was a retrospective, single-center cohort study of HIE neonates (gestational age ≥ 36 weeks) who underwent TH between January 2012 and December 2022. Neonates with other significant congenital anomalies, genetic conditions, need for extracorporeal membrane oxygenation, or in-hospital mortality were excluded. Following rewarming, a modified barium swallow (MBS) was performed on neonates considered at risk for aspiration to identify swallowing impairment; brain MRI was performed in clinically stable babies (usually between 5-7 days of life). EEG was continuously performed from TH initiation till at least 80 hours of life.
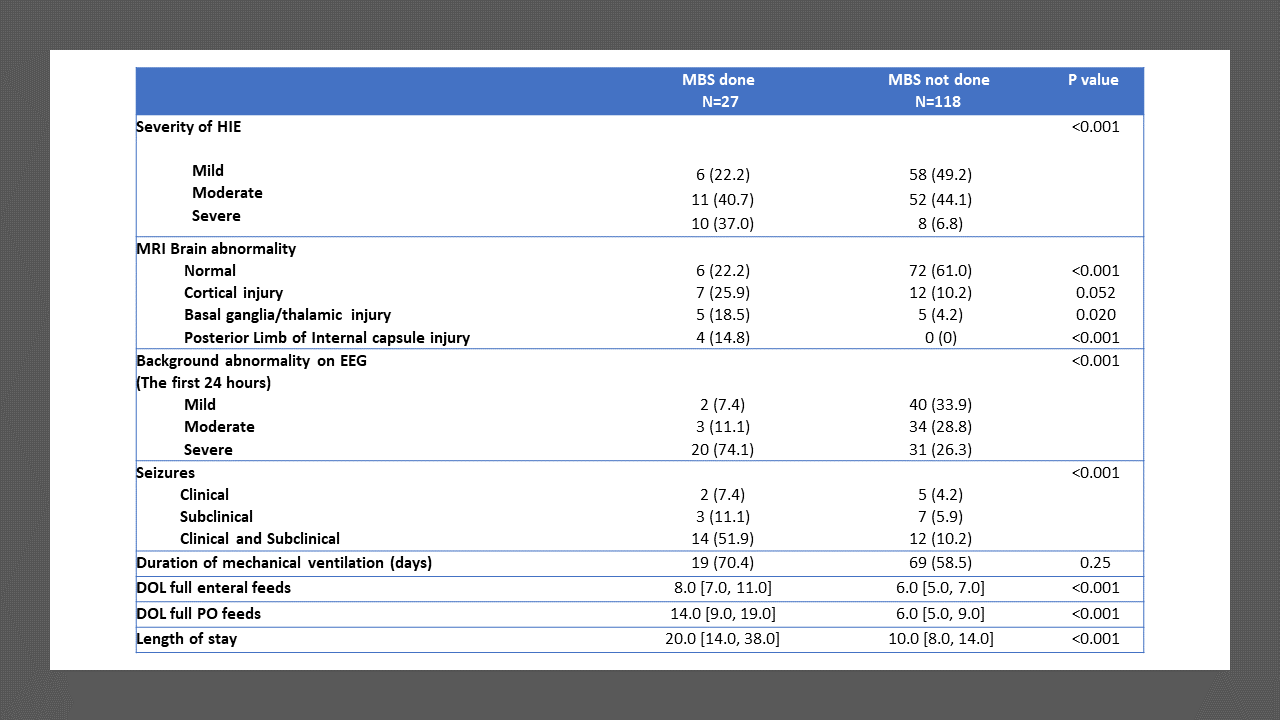
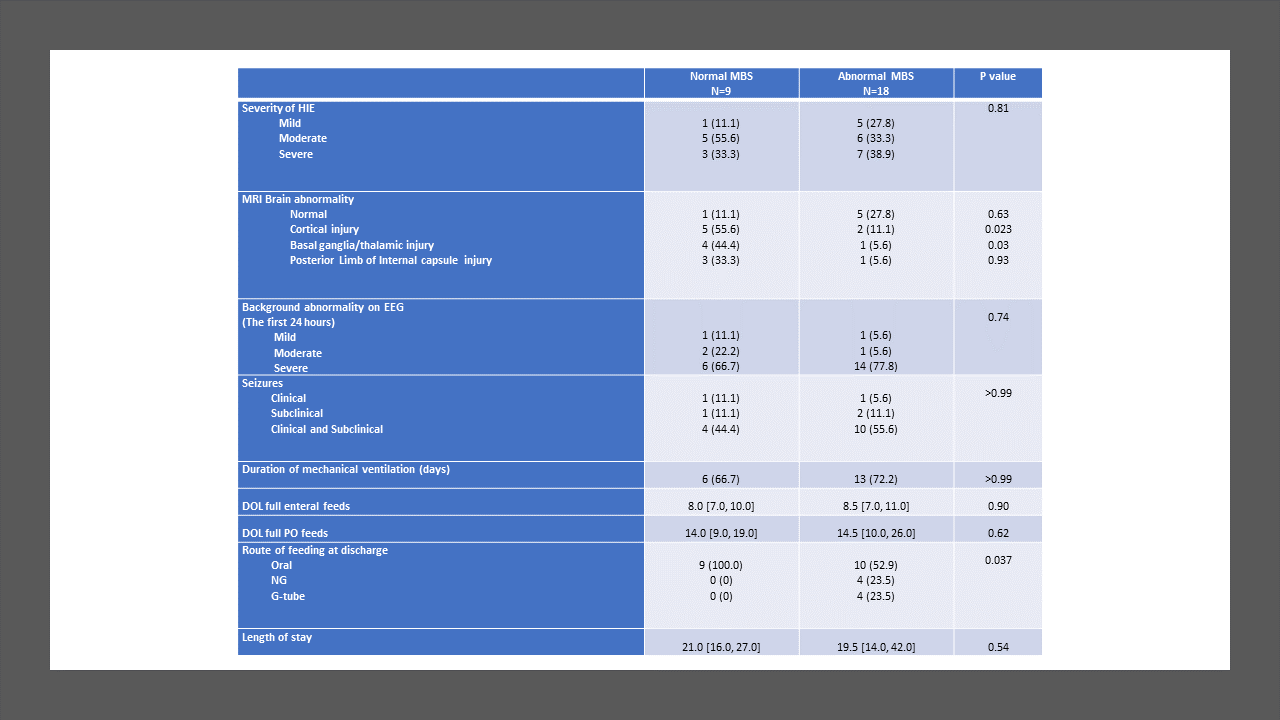
Results: In total, 145 neonates were included, with 55.9% males, 59.3% born by cesarean section, and 43.4/12.4% moderate/severe HIE. Median gestational age was 39.3 weeks. Overall, 27/145 (18.6%) MBS evaluations were performed: 9 (33.3%) normal, 8 (29.6%) dysphagia without aspiration, and 10 (37.0%) dysphagia with aspiration. Prevalence of abnormal swallow study was 7/18 (39%) in severe HIE, 6/63 (9%) in moderate HIE and 5/64 (8%) in mild HIE. Infants who required MBS had a significantly higher incidence of seizures, abnormal MRI, EEG, and longer hospital stay. Infants with abnormal MBS had more cortical, basal/thalamic ganglia injury compared to neonates with normal MBS. Among the infants who had abnormal MBS, only 8/18 (44 %) were discharged home on tube feeds: 4 with nasogastric and 4 with gastrostomy tube.
Conclusion(s): In this cohort of babies with HIE treated with TH, the prevalence of dysphagia was lower (overall 12.4%) than previously reported. Dysphagia improved in most babies by the time of discharge. Infants who required MBS had a significantly higher incidence of abnormalities on MRI. MBS should be limited to the babies with moderate to severe HIE.