Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
84 - ST Segment Variability is Associated with Presence of High Volume Patent Ductus Arteriosus Shunt in Extremely Low Birth Weight Infants
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 84
Publication Number: 84.2203
Publication Number: 84.2203

Danielle R. Rios, MD, MS (she/her/hers)
Associate Professor of Pediatrics
University of Iowa Department of Pediatrics
Iowa City, Iowa, United States
Presenting Author(s)
Background: ST segment changes on electrocardiogram are routinely utilized in adults to evaluate for ischemic changes in cardiac muscle but are rarely monitored in the NICU. In the congenital heart disease population, ST segment variability has been associated with cardiopulmonary arrest in neonates with single-ventricle physiology. Extremely preterm infants with hemodynamically significant patent ductus arteriosus (hsPDA) are at risk of coronary artery ischemia due to low diastolic aortic pressure with reports of elevated troponin. A correlation between ST segment changes and hsPDA in preterm infants has yet to be investigated clinically.
Objective: To evaluate the degree of correlation between ST segment variability and presence of hsPDA in a cohort of premature infants.
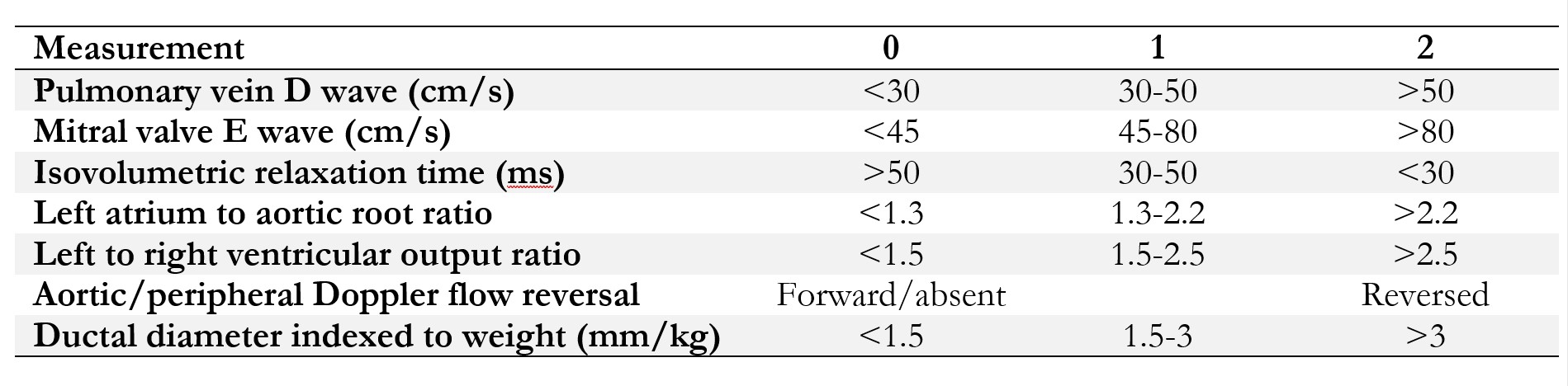
Design/Methods: Data were prospectively collected 6/20-2/22 from inborn patients (birth weight ≤1000g and gestational age < 29 weeks) enrolled in a clinical trial at the University of Iowa; ST segments from leads I, II, III, and aVF were collected for the first postnatal week using the Sickbay software platform allowing for retrospective analysis. All patients underwent targeted neonatal echocardiography (TnECHO) at least once as part of the research protocol. Patients were excluded for life-threatening congenital defect or chromosomal abnormality, congenital hydrops, compromised skin integrity, or in extremis. TnECHOs were excluded if they had abnormal heart function. The Iowa PDA score (Table 1) was calculated for all TnECHOs obtained during the one-week study period. The distribution of ST segment variability was compared in patients with high-volume (PDA score ≥9) vs. low-volume shunt (PDA score ≤2 or no PDA) using Wilcoxon rank-sum test. A p-value of < 0.05 was used for significance.
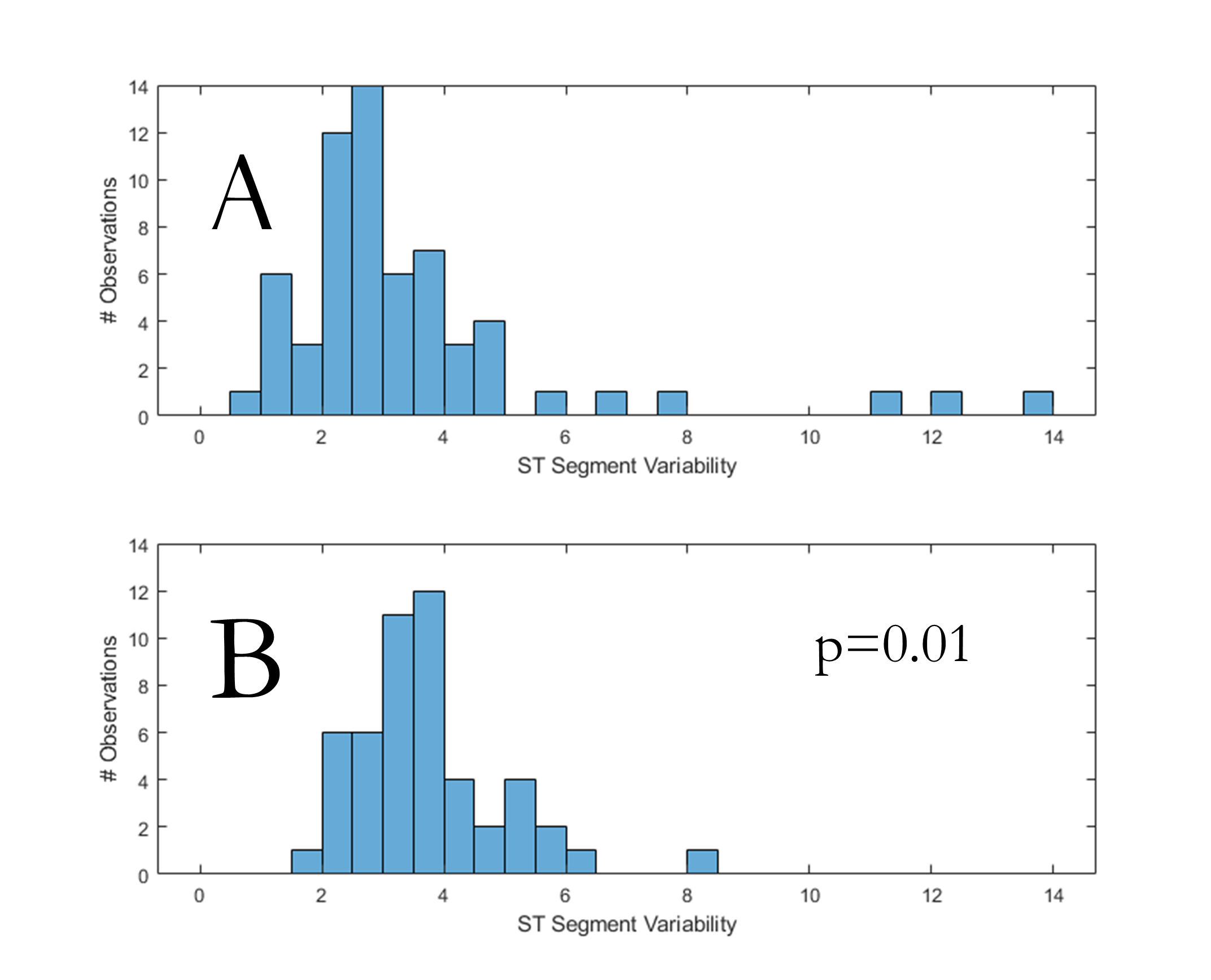
Results: A total of 139 TnECHOs from 54 patients with mean birth weight and gestational age 703 ± 157 grams and 25.1 ± 1.7 weeks, respectively, were evaluated for inclusion. Of those, 12 TnECHOs had findings consistent with high-volume and 48 with low-volume shunt and were included in the analysis. The median (IQR) distribution of ST segment variability in patients with high-volume shunt [3.52 (2.91, 4.14)] was greater (p=0.01) than those with low-volume shunt [2.91 (2.08, 3.74)]. The influence of potentially confounding variables (heart rate, diastolic blood pressure, pO2, pCO2) is being investigated.
Conclusion(s): In extremely low birth weight infants, increased ST segment variability was associated with a high-volume shunt from hsPDA. The impact of myocardial instability on short-term clinical stability and heart development requires prospective evaluation.
.jpg)
