Emergency Medicine
Session: Emergency Medicine 8: Mental Health
588 - Outcomes of Children and Adolescents in Acute Psychiatric Crisis Treated in a Pediatric Observation Unit versus Admission to an Inpatient Psychiatric Unit
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 588
Publication Number: 588.2181
Publication Number: 588.2181
.jpg)
Rachel G. Kasdin, M.S. (she/her/hers)
Medical Student
Icahn School of Medicine at Mount Sinai
New York, New York, United States
Presenting Author(s)
Background: Pediatric emergency departments (PED) are increasingly relied upon for the management of acute mental health concerns. Pediatric observation units (POU) can provide ongoing care to children requiring psychiatric admission. There is limited understanding regarding the impact of pediatric observation units (POU) have on PED utilization, length of stay (LOS) and outcomes in patients with psychiatric complaints.
Objective: To identify variables impacting LOS and disposition between patients admitted directly to an inpatient unit and patients admitted first to POU.
Design/Methods: This study utilized a retrospective cohort design at two PEDs in an urban, academic healthcare system, one of which has a POU offering ongoing psychiatric co-management, which includes monitored medication adjustment, social work and case management, and child-life services; only case management is available to patients at the site without a POU. Inclusion criteria were age <=18 y.o. with an initial decision to admit to an inpatient psychiatric unit from January-June 2022. Charts were reviewed and patient demographics, PED and POU course if applicable, and disposition were collected. Primary outcome is the rate of completed admission and LOS to an inpatient psychiatric unit between the POU group and comparison group.
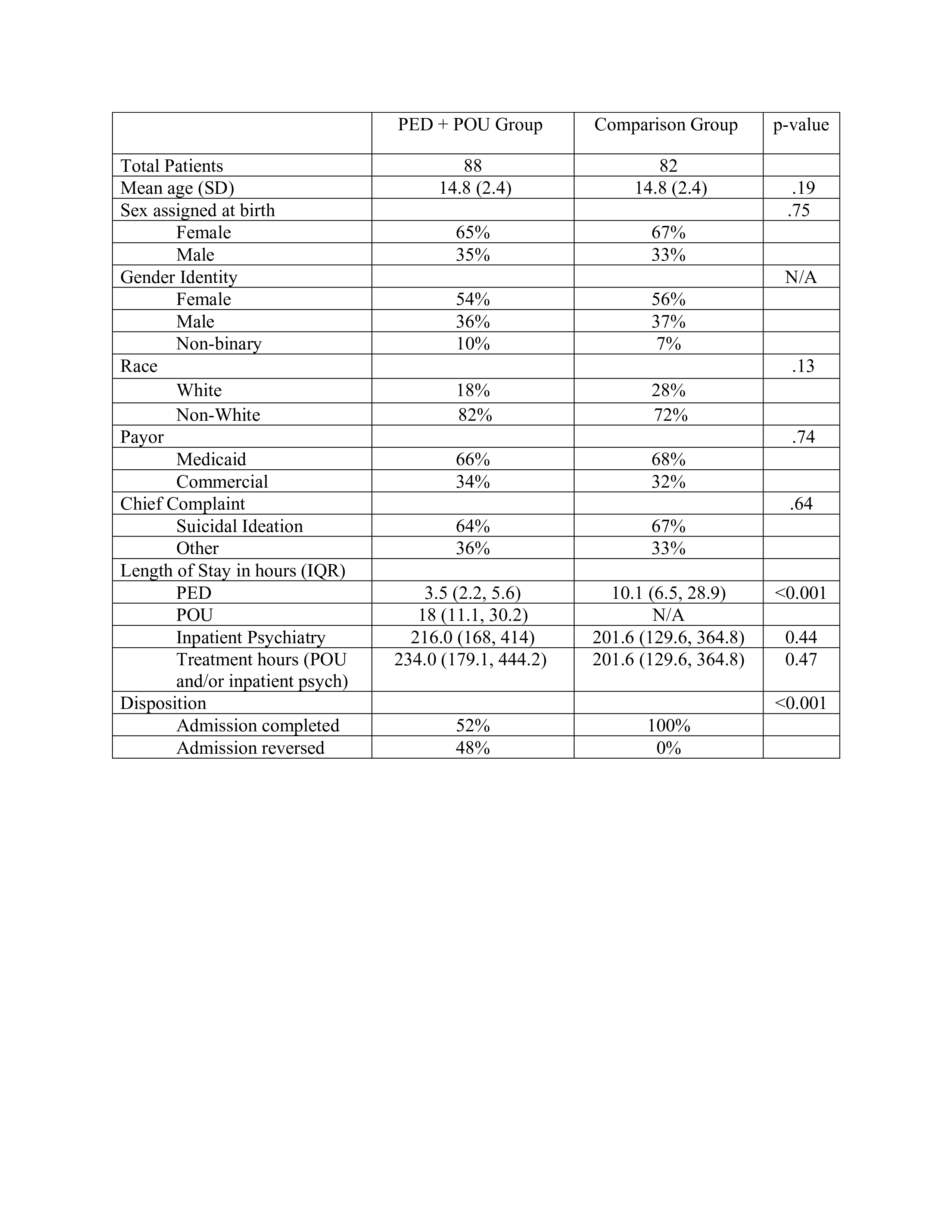
Results: Patient characteristics and treatment courses for those meeting the inclusion criteria at each site are listed in Table 1. There were no significant differences between groups with regards to age, sex, gender, race, payor, and chief complaint. There was a significant difference in PED LOS between sites (p < 0.001); there was no significant difference in treatment hours (POU+inpatient) between sites (p=0.47) or inpatient LOS (p=0.44). Of the patients at the site with a POU, 48% had their admission decision reversed. Of the patients in the PED site without a POU, no patient admission decisions were reversed. Patients at the site with a POU were 1.9 times less likely to require admission to an inpatient psychiatric unit (95% CI 1.6-2.3).
Conclusion(s): Psychiatric co-management in a POU may decrease the burden of care in the PED and reduce the need for inpatient admission among children with psychiatric emergencies. POUs may be able to address patient and system needs amidst rising rates of youth psychiatric distress.