Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 1
362 - Pediatric Critical Care Provider Sign Out Quality Improvement
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 362
Publication Number: 362.2150
Publication Number: 362.2150

Kevin D. Smith, MD, MS (he/him/his)
Clinical Informatics Fellow
Comer Children's Hospital at University of Chicago Medical Center
Willowbrook, Illinois, United States
Presenting Author(s)
Background: Handoffs between providers caring for pediatric intensive care unit (PICU) patients are critical to longitudinal patient care. Communication failures during provider handoffs are common for various reasons, including the complexity of patients, interruptions to the sign out process, and varying degrees of sign out & clinical experience, particularly with trainees.
Objective: We report a quality improvement project to improve the accuracy of handoff information, decrease interruptions to the sign out process, and decrease the total time spent signing out.
Design/Methods: We surveyed PICU providers (attendings, fellows, and advance practice nurses) about estimated time spent signing out, appropriateness of sign out time/content, and barriers to effective sign out. We then performed an observational time series at an academic PICU between April 2023 and June 2023. After collecting pre-intervention data, process changes were implemented using three plan-do-study-act (PDSA) cycles. We also surveyed providers twice daily immediately after sign out, asking whether they were “satisfied” with the most recent instance of handoff.
Results: The response rate to our survey was 46%. 58% of respondents stated that the time spent signing out was “rarely” appropriate. Information was provided in “too much detail” for 83% of respondents. However, 67% of providers stated that important details were missed at least a few times per week. The most frequent barriers to effective sign out were “outside interruptions” (83%), “variability in receiving provider preferences” (75%), and “new provider unfamiliar with current patients” (67%).
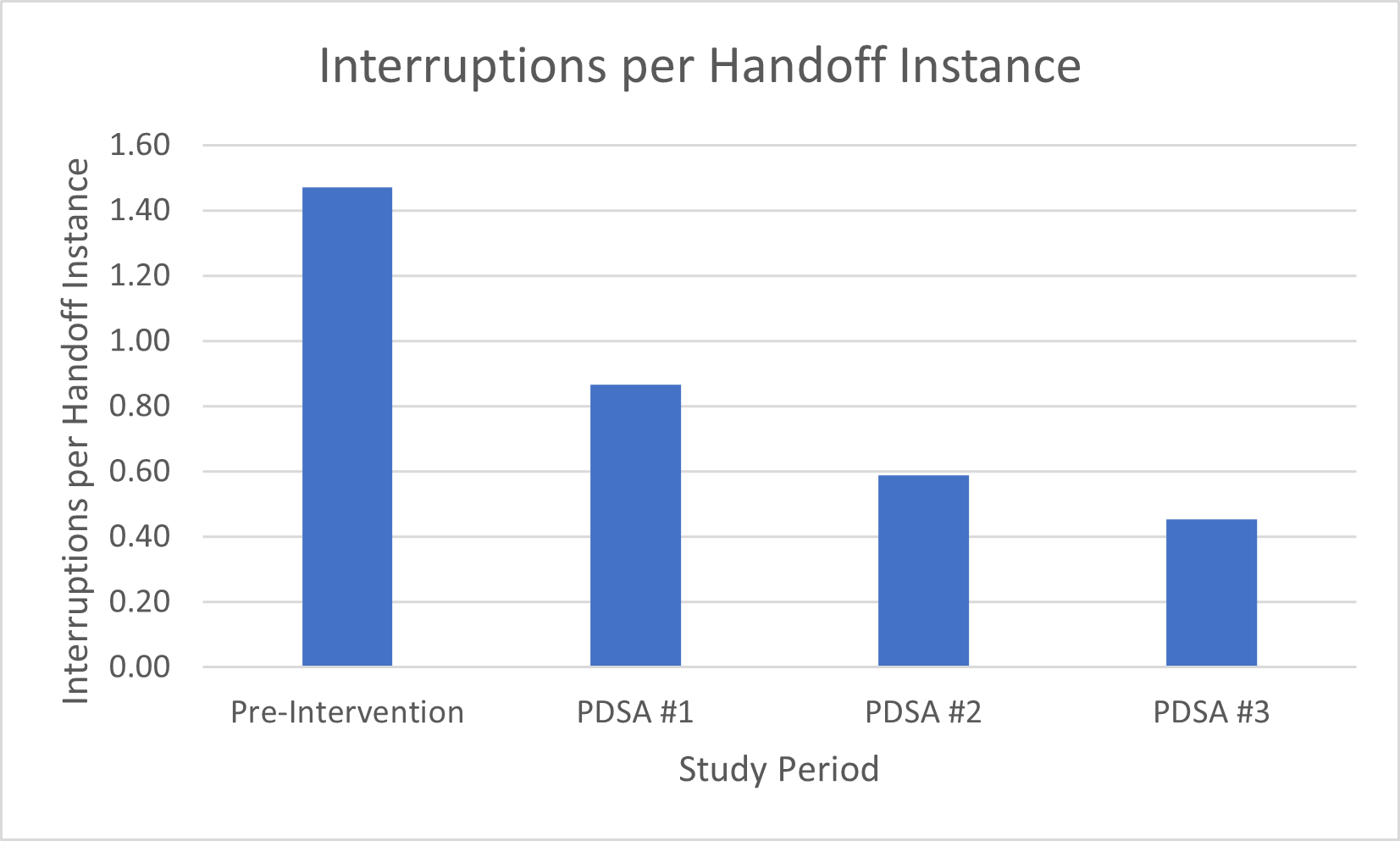
In the first PDSA cycle, we hung a “stop” sign outside the provider workroom to discourage non-urgent interruptions. For PDSA cycle #2, we instituted a hand off agenda with ground rules and provided a sign out template for providers to follow. In our last PDSA cycle, we sent messages to team members not signing out (e.g., nurses and resident physicians) asking them to hold non-urgent questions until after handoff was completed.
Interruptions to the handoff process decreased by 69% from the pre-intervention to the end of cycle #3. The total time signing out decreased by 30% during the same period, but time spent signing out per patient only decreased by 2%.
Before our PDSA cycles, providers were satisfied with individual sign out instances 91% of the time. By the completion of PDSA cycle #3, that increased to 93% of the time.
Conclusion(s): Process changes led to a significant reduction in interruptions to provider handoff, along with a reduction in total time spent signing out.