Neonatology
Session: Neonatal Pulmonology - Clinical Science 1: BPD, BPD Biomarkers and Diagnosis
191 - Synergistic effects of perinatal interventions on bronchopulmonary dysplasia or death in preterm infants born less than 28 weeks’ gestational age
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 191
Publication Number: 191.2982
Publication Number: 191.2982

Xiang Chen, PhD
Shanghai
Children's Hospital of Fudan University
Shanghai, Shanghai, China (People's Republic)
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD), mainly caused by the disruption of pulmonary alveolarization and vascularization, is one of the major prematurity-related complications. Data-driven quality improvement in preventing BPD in CHNN is urgent.
Objective: To investigate the effect of perinatal interventions on the risk of severe BPD (sBPD) or death in extremely preterm infants and their synergistic effects.
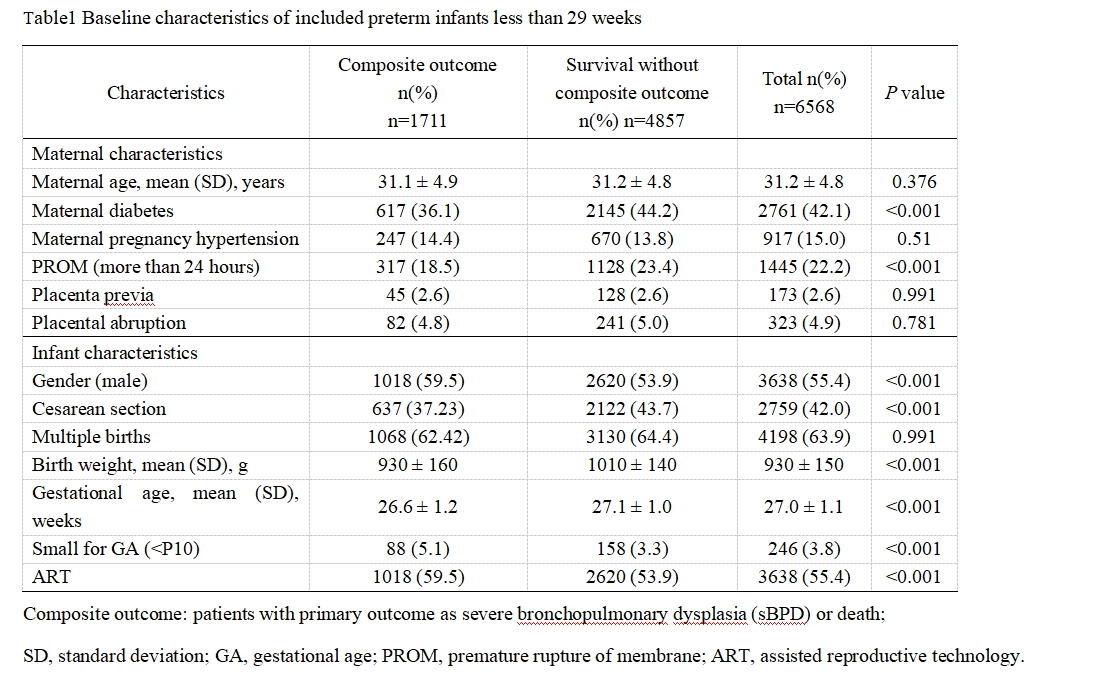
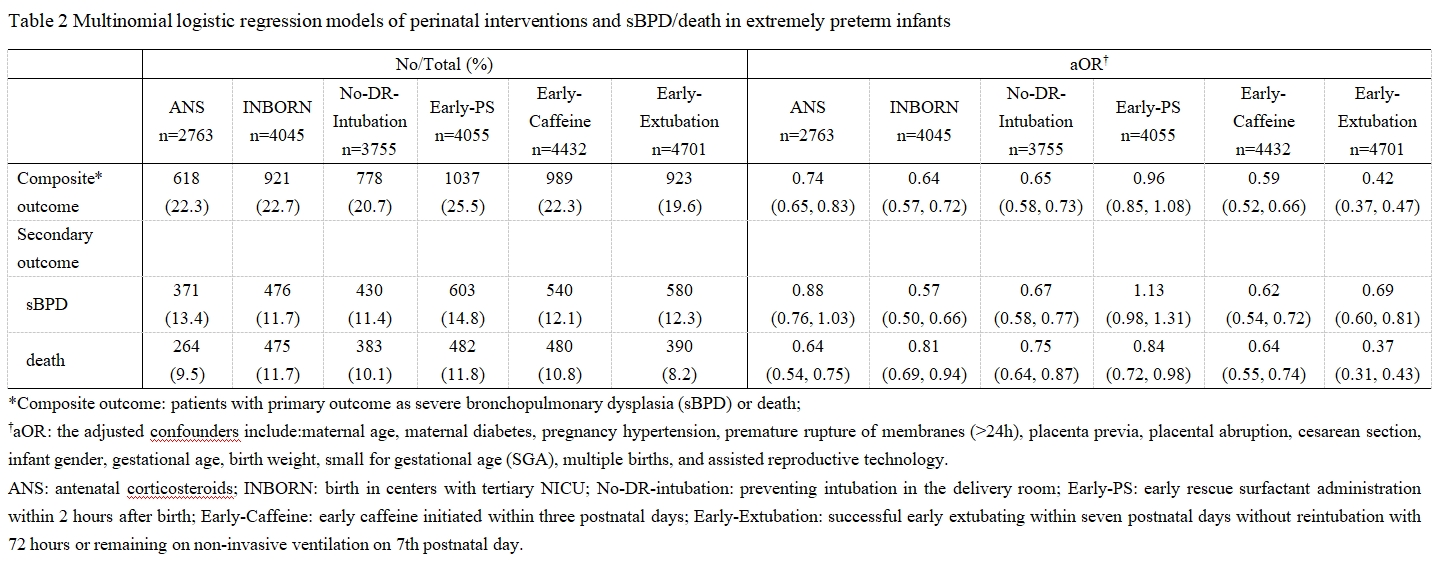
Design/Methods: This is a retrospective cohort study. From 2019 to 2021, infants with 24-28 weeks completed gestational age were recruited from the Chinese Neonatal Network (CHNN). The impacts and the synergistic effects of six selected perinatal interventions on the composite primary outcomes of severe BPD (sBPD) or death were assessed by univariate and multivariable logistic regression modeling. Six interventions included antenatal corticosteroids (ANS), birth in centers with tertiary NICU (INBORN), preventing intubation in the delivery room (No-DR-intubation), early rescue surfactant administration within 2 hours after birth (Early-PS), early caffeine initiated within three postnatal days (Early-Caffeine), and successful early extubating within seven postnatal days without reintubation with 72 hours or remaining on non-invasive ventilation on 7th postnatal day (Early-Extubation). Severe BPD and death were individually set as secondary outcomes.
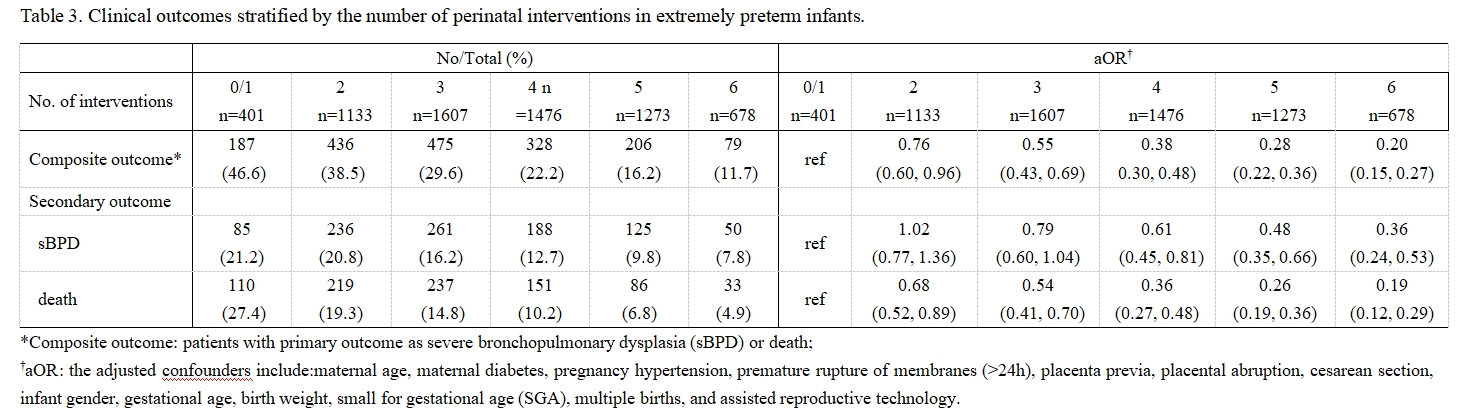
Results: Totally, 6568 infants were finally enrolled. Antenatal corticosteroid (adjusted OR, aOR, 0.74; 95%CI, 0.65-083), birth in centers with tertiary NICU (aOR, 0.64; 95%CI, 0.57-0.72), preventing intubation in the delivery room (aOR,0.65; 95%CI, 0.58-0.73), early caffeine therapy (aOR, 0.59; 95%CI, 0.52-0.66), and early extubating (aOR, 0.42; 95%CI 0.37-0.47), were strongly associated with a lower risk of composite primary outcome while early surfactant administration was associated with a lower risk of death (aOR, 0.84; 95%CI, 0.72, 0.98). Compared with achieving 0/1 perinatal interventions, achieving more than one intervention was associated with decreased rates (46.6% in 0/1 groups while 38.5%, 29.6%, 22.2%, 16.2%, 11.7% in 2/3/4/5/6-intervention groups respectively) and reduced risks of composite primary outcome with aORs of 0.76(0.60, 0.96), 0.55(0.43, 0.69), 0.38(0.30, 0.48), 0.28(0.22, 0.36), and 0.20(0.15, 0.27) in 2, 3, 4, 5, 6-intervention groups respectively. Subgroup analyses showed consistent results.
Conclusion(s): Evidence-based perinatal interventions can effectively reduce the risk of sBPD or death in a synergistic form.