Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
375 - Quality Improvement Initiatives Decrease the Age at Autism Spectrum Disorder Diagnosis and Early Intervention in a High Risk Infant Follow Up Program
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 375
Publication Number: 375.2024
Publication Number: 375.2024

Alyssa E. Blumenfeld, MD, MS (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Early diagnosis and intervention improves outcomes for children with autism spectrum disorder (ASD). Infants born preterm or requiring NICU admission are at significantly higher risk for developing ASD and are also disproportionately affected by pre- and post-natal healthcare disparities. As such, high-risk infant follow-up (HRIF) clinics are an important setting to implement early detection and referral for ASD services.
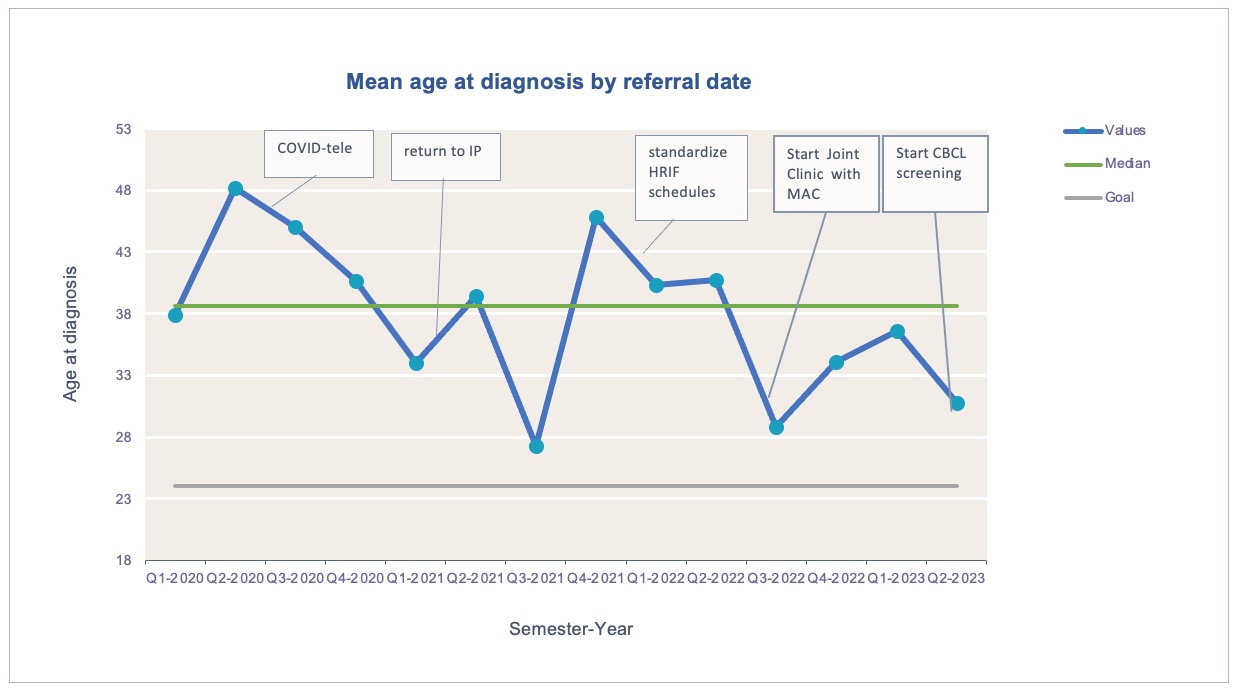
Objective: To decrease the average age at autism diagnosis in an HRIF to 26 months corrected age by July 2024 through sequential implementation initiatives.
Design/Methods: We leveraged improvement tools (key driver diagrams and PDSA cycles), and LEAN methodology (process flow analysis and waste walks) to change clinic procedures and ASD referrals in a large HRIF regional program. We conducted three overarching PDSA cycles with smaller refinements of the main intervention in each cycle. Cycle 1: 11/2021-8/2022, we standardized all clinic schedules, visit content and referral algorithms from 3 months to 5 years. Cycle 2: 11/2022-8/2023 we partnered with the Marcus Autism Center to create a weekly joint clinic facilitating referrals. Cycle 3 9/2023-present, we implemented systematic screening for all 18-26 month visits using the withdrawn and pervasive developmental disorder scales of the child behavior checklist (CBCL).
Results: From 2020 to 2023, the average age at ASD diagnosis decreased from 41 months at baseline to 38.6 in Cycle 1 and 33.6 in Cycle 2 (Figure 1). This was driven by a process measure: wait time between referral for ASD evaluation and ASD diagnosis- which decreased from 9.6 months at baseline to 6.2 (Cycle 1) to 2.9 (Cycle 2) (Figure 2). The number of new diagnoses increased from 16 in 2020 to 41 in 2022, likely due to delays during the COVID-19 pandemic but stabilized in 2023. As our HRIF screens for social determinants of health, no differences were noted in age at diagnosis between black and white children. Finally, our balancing measure of age at early intervention also decreased from 38 months at baseline, to 32.4 in Cycle 1 and 27.2 in Cycle 2. Cycle 3 results are still pending but are trending toward our stated aim.
Conclusion(s): While our implementation initiatives decreased age at ASD diagnosis, we have not yet reached our stated aim. Given the demonstrated benefits of early diagnosis and early intervention for ASD to children, families, social, and healthcare systems, it is critically important to continue implementing systemic changes to HRIF and partnering across pediatric disciplines.
.jpg)
