Health Services Research
Session: Health Services Research 4: Population Monitoring and Management
249 - Association Between Telehealth Initiation of Stimulant Therapy During the COVID-19 Pandemic and Substance Use Disorders Among U.S. Adolescents and Young Adults
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 249
Publication Number: 249.1981
Publication Number: 249.1981

Joanne Constantin, PhD (she/her/hers)
Postdoctoral Research Fellow
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: During the COVID-19 pandemic, policymakers allowed stimulant prescribing via telehealth without in-person visits. Concerns about inappropriate prescribing in telehealth visits have sparked debates on whether this policy should be extended.
Objective: To inform these debates, we assessed the association between telehealth initiation of stimulant therapy during the pandemic and both prior and new substance use disorders (SUDs) among adolescents and young adults (AYAs) with ADHD.
Design/Methods: Using the Merative MarketScan Commercial and Multi-State Medicaid Databases, we identified AYAs aged 12-25 years initiating therapy with methylphenidate or amphetamine during March 1, 2020-June 30, 2021. We limited to AYAs with an in-person or telehealth visit for ADHD in the 3 days prior to dispensing. The exposure was telehealth initiation. Outcomes were prior SUD (any SUD diagnosis in the 180 days before initiation) and new SUD (any SUD in the 180 days after initiation among those without prior SUD). We used logistic regression to model outcomes as a function of the exposure, payer type, and their interaction, controlling for age, sex, and year-month. For each payer type, we calculated average marginal effects (AMEs), the absolute percentage-point (pp) change in the risk of the outcome if all versus no patients initiated stimulants via telehealth. We calculated the difference in AMEs by payer type to assess for effect modification.
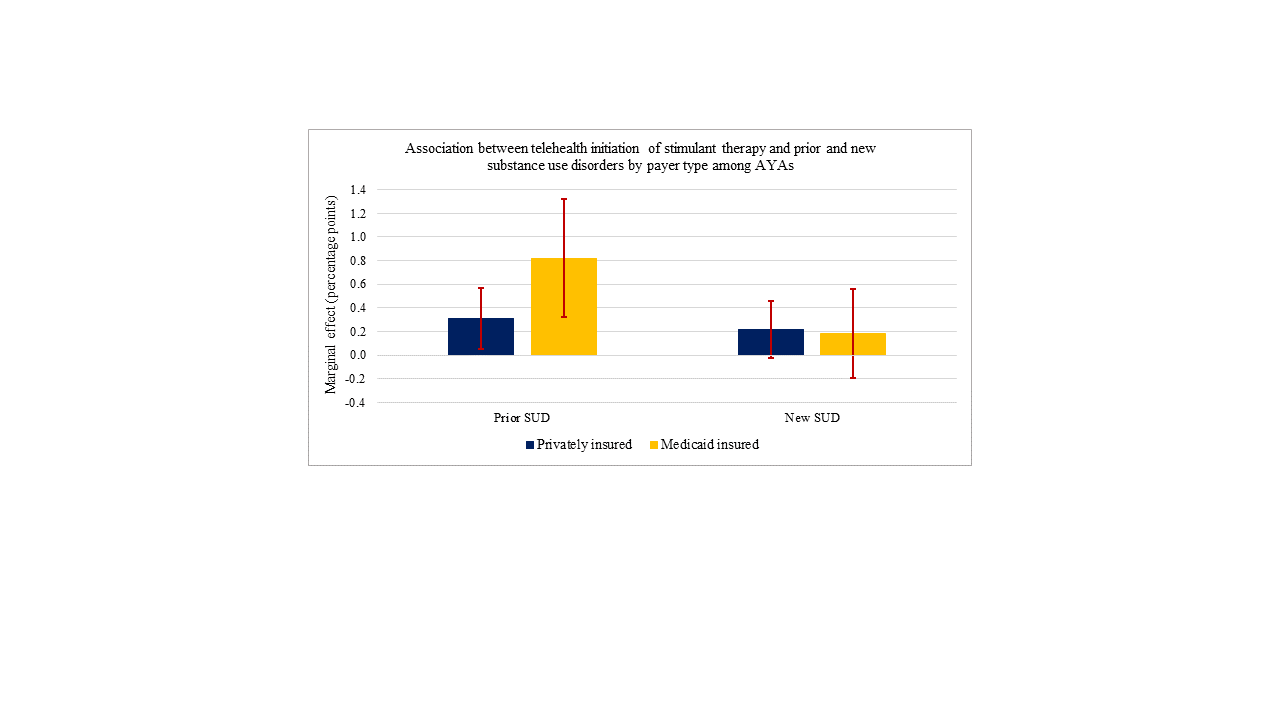
Results: Of 39,123 privately insured and 39,866 Medicaid patients included, 33.1% and 27.8% had a telehealth visit in the prior 3 days. Among privately insured AYAs, the risk of prior SUD in the telehealth and in-person group was 3.4% and 2.5% (AME: 0.3 pp, 95% CI: 0.05, 0.6), compared with 3.3% and 2.4% among Medicaid-insured AYAs (AME: 0.8 pp, 95% CI: 0.3, 1.3; difference in AMEs: 0.5 pp, 95% CI: -0.05, 1.1). Among privately insured AYAs, the risk of new SUD in the telehealth and in-person group was 2.3% and 1.8% (AME: 0.2 pp, 95% CI: -0.03, 0.5), compared with 2.0% and 1.8% among Medicaid-insured AYAs (AME: 0.2 pp, 95% CI: -0.2, 0.6; difference in AMEs: -0.03 pp, 95% CI: -0.5, 0.4; Figure).
Conclusion(s): If telehealth flexibilities for controlled substance prescribing are extended, clinicians should screen AYAs for prior SUDs before initiating stimulants for ADHD via telehealth. Although telehealth stimulant initiation was not associated with a higher adjusted risk of new SUD, the unadjusted risk was higher in both payer populations. Thus, screening for new SUDs among AYAs who initiate stimulant therapy via telehealth may also be needed.