Neonatology
Session: Neonatal Neurology 4: Clinical
530 - Sleep State Differences in Cerebral and Arterial Oxygenation and Cardiac Activity in Preterm Infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 530
Publication Number: 530.1408
Publication Number: 530.1408
.jpg)
Toni P. Iurcotta, MD (she/her/hers)
Clinical Fellow
NewYork-Presbyterian Morgan Stanley Children's Hospital, Columbia University Medical Center
New York, New York, United States
Presenting Author(s)
Background: Cerebral regional oximetry (C-rSO2) provides a weighted average of the venous, arterial, and capillary saturations, and together with pulse oximetry-derived arterial oxygenation (SpO2), it can estimate local O2 demand and consumption. However, there is a paucity of information on cerebrovascular control during various sleep states in preterm infants.
Objective: To evaluate sleep state differences in C-rSO2, SpO2 and heart rate (HR), and whether a multimodal sensory stimulation mimicking the intrauterine environment could influence these differences in preterm infants.
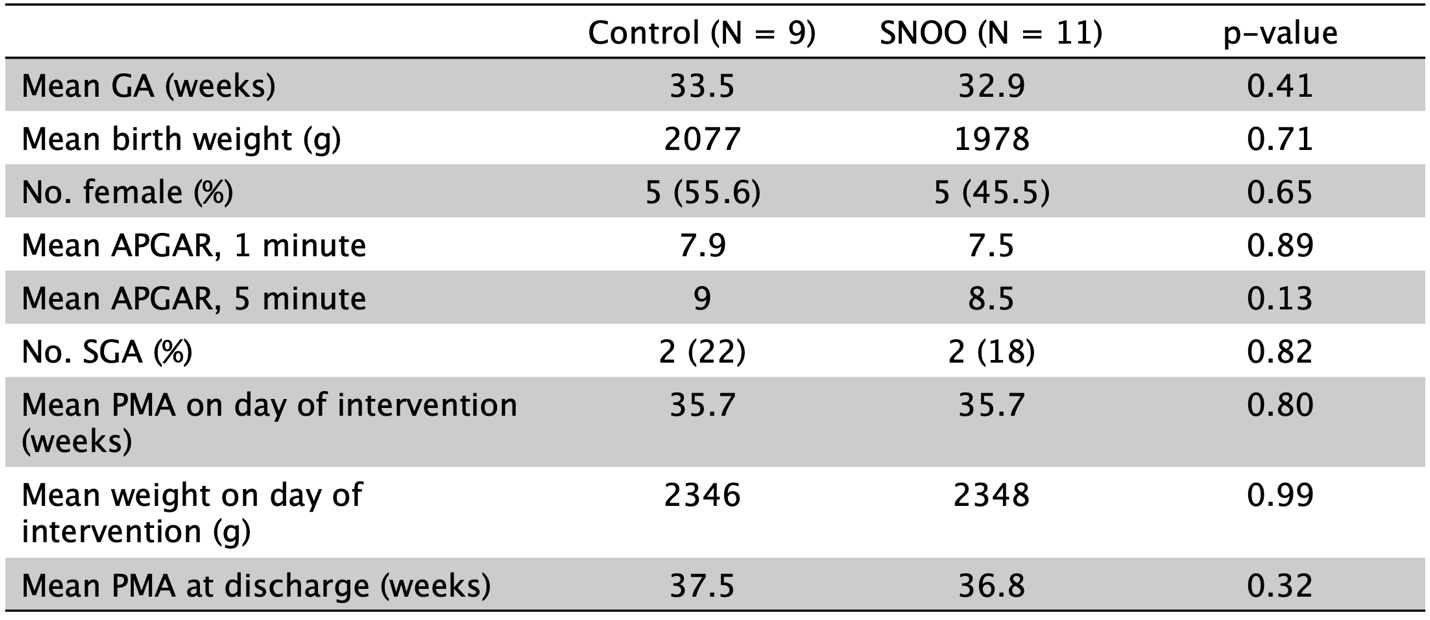
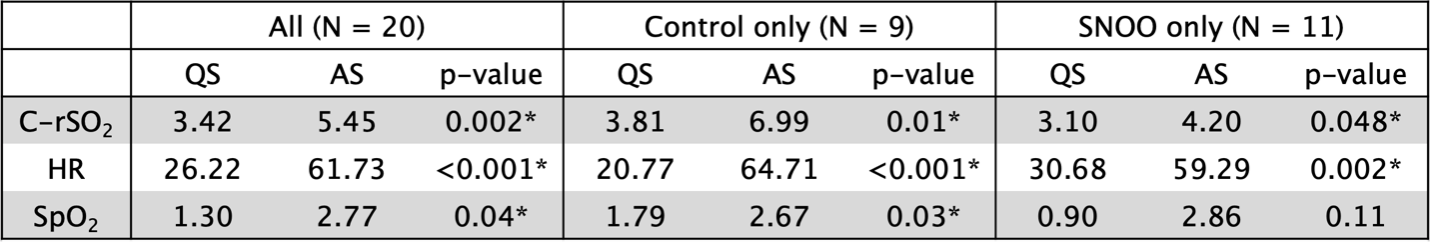
Design/Methods: A prospective randomized controlled study was performed in 20 preterm infants born between 28-36 weeks postmenstrual age (PMA) and admitted to a level IV NICU. When infants reached 35-36 weeks PMA, weighed >1.8 kg, and were off respiratory support in open cribs, they were randomized to be placed in a bassinet (SNOO Smart Sleeper) that combined rocking, swaddling, and white noise or in a powered-off bassinet (control) for a single 2-3-hour interfeed period of continuous monitoring of C-rSO2, SpO2 and HR, along with min-to-min assessment of behavioral states (quiet sleep (QS); indeterminate sleep (IS); active sleep (AS); awake; and crying) using a validated scoring system. Pooled coefficients of variation (CV) for C-rSO2, SpO2, and HR during QS and AS were compared across all infants and between the SNOO and control groups using Student’s t-tests.
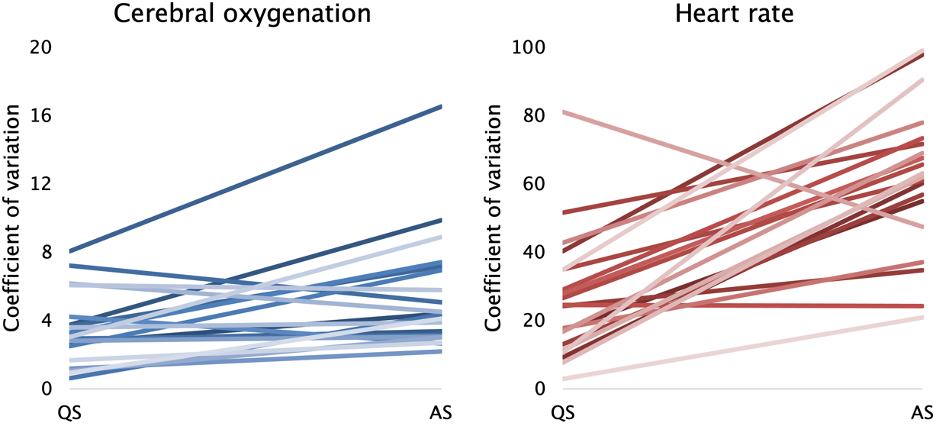
Results: The SNOO and control groups of infants had similar characteristics (Table 1). Across all infants, QS was associated with lower CV for C-rSO2 (3.42 vs. 5.45%, p=0.002), SpO2 (1.3 vs. 2.77%, p=0.04), and HR (26.22 vs. 61.73 bpm, p< 0.001) as compared to AS (Table 2). In control infants, the CV of C-rSO2 (3.81 vs. 6.99%, p=0.01), SpO2 (1.79 vs 2.67%, p=0.03), and HR (20.77 vs. 64.71 bpm, p< 0.001) were again lower during QS than in AS. In SNOO infants, the CV of C-rSO2 (3.1 vs. 4.2, p=0.048) and HR (30.68 vs. 59.29, p=0. 002) were lower during QS than in AS, with a nonsignificant trend towards lower CV of SpO2 in QS (0.9 vs 2.86%, p=0.11).
Conclusion(s): Preterm infants demonstrated decreased variability in C-rSO2, SpO2, and HR during QS compared to AS. Multimodal sensory stimulation led to lower variabilities during QS, but the QS/AS differences were attenuated compared to controls. These data suggest that QS and AS differences in cerebral oxygenation and hemodynamics can be influenced by a brief exposure to a multimodal sensory stimulation. Whether these autonomic adjustments persist with prolonged exposure and can modulate sleep and clinical outcomes needs to be evaluated.