Neonatology
Session: Neonatal Neurology 2: Clinical
27 - Predictive Ability of Amplitude Integrated Electroencephalography for Adverse Outcomes in Neonates with Sepsis-Associated Encephalopathy: A Cohort Study
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 27
Publication Number: 27.295
Publication Number: 27.295

Shiv Sajan Saini, D.M. (Neonatology), MD (Pediatrics) (he/him/his)
Associate Professor
Post Graduate Institute of Medical Education and Research
Chandigarh, Chandigarh, India
Presenting Author(s)
Background: Sepsis-associated encephalopathy (SAE) is defined as an altered mental status in the presence of sepsis, without evidence of direct CNS infection. The spectrum of amplitude-integrated electroencephalography (aEEG) abnormalities in neonates with SAE is currently unknown.
Objective: To examine the prevalence of severely abnormal aEEG patterns in neonates suffering from SAE and investigate the predictive ability of aEEG for adverse outcomes
Design/Methods: We enrolled neonates with culture-proven or probable sepsis, who had encephalopathy as per the Brighton Collaboration Neonatal Encephalopathy Working Group criteria, and a normal CSF examination. We excluded neonates with known etiologies of neonatal encephalopathy. We recorded their aEEG for 6-12 hours. The aEEG patterns were identified using Hellström-Westas criteria. Two independent blinded reviewers assigned Burdjalov scores, and sleep-wake cycle patterns. We assessed their neurological examinations before discharge using the Amiel-Tison assessment tool. Our primary outcome was death or abnormal neurological findings at discharge.
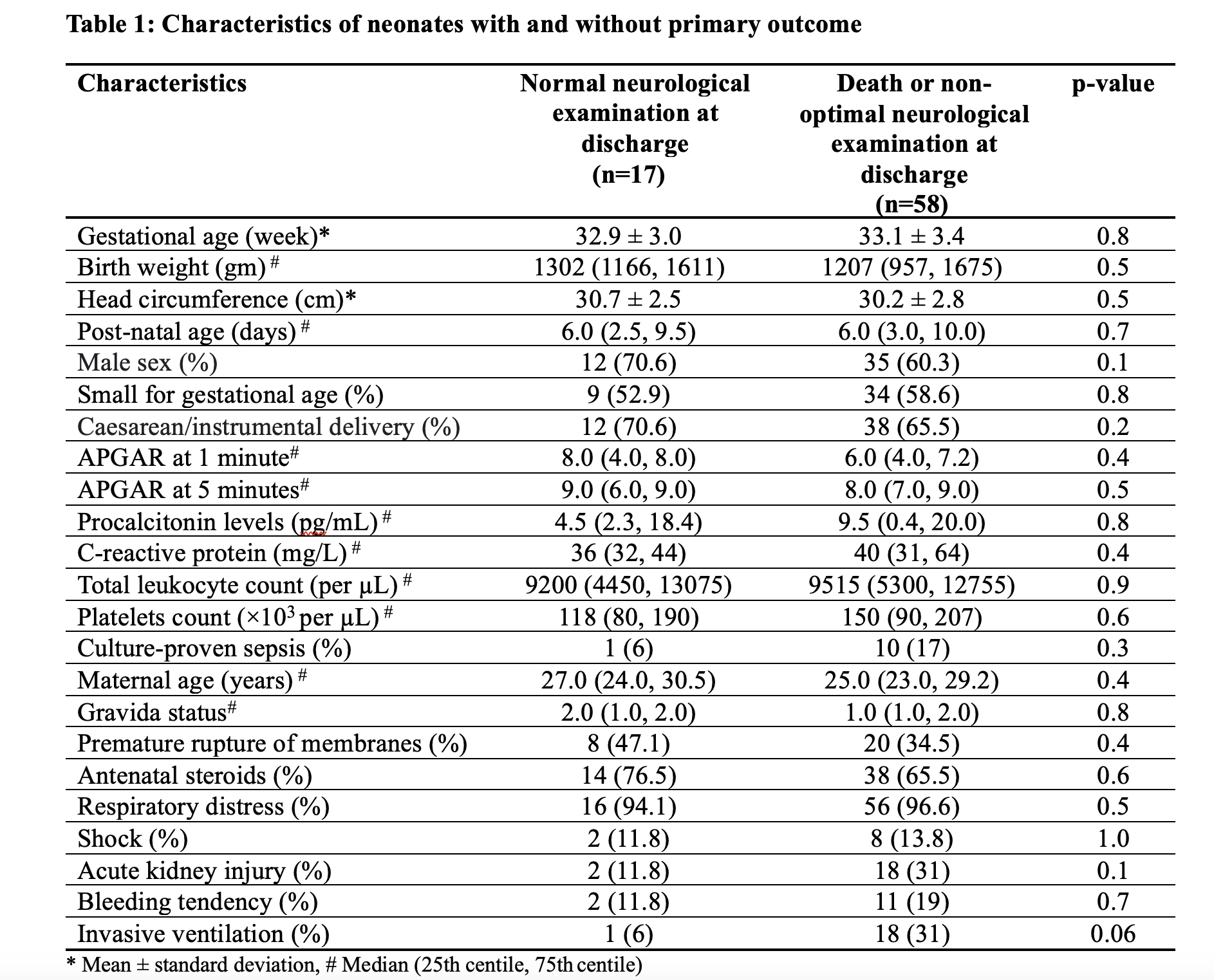
Results: We recorded 36,626 minutes of aEEG from 75 neonates with SAE. The prevalence of severely abnormal patterns ( isoelectric voltage, continuous low voltage, burst suppression) was 31%. Of the 75 neonates, 58 (77%) experienced the primary outcome [died (n=12), left against medical advice with neurological abnormalities (n=5), abnormal neurological examination at discharge (n=41)]. Baseline characteristics of neonates who experienced and those who did not experience the primary outcome were comparable (Table 1). Neonates who experienced the primary outcome had a significantly higher prevalence of severely abnormal aEEG patterns, worse Burdjalov scores, and abnormal sleep-wake cycles compared to survivors with normal neurological examinations. ROC curve analysis revealed that the Burdjalov score had a statistically significant area under the curve [0.69 (95% CI: 0.53, 0.85), p- 0.02] to discriminate the primary outcome. After adjusting for gestational age, birth weight, and invasive ventilation, severely abnormal aEEG (OR 5.8, 95% CI 1.7-19.5, p-value 0.005) and Burdjalov scores (OR 0.77, 95% CI 0.63-0.95, p-value 0.01) were independently associated with death or abnormal neurological findings at discharge.
Conclusion(s): Neonates with SAE had 31% prevalence of severely abnormal aEEG patterns, which were significantly associated with an increased risk of mortality or abnormal neurological findings at discharge. Abnormal aEEG patterns and Burdjalov scores can independently predict adverse outcomes in neonates with SAE.