Neonatology
Session: Neonatal Clinical Trials 1
473 - Hospital Care Settings for Pharmacologically Treated Infants in the ESC-NOW Randomized Controlled Trial
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 473
Publication Number: 473.1656
Publication Number: 473.1656
Hellen Ko, MD (she/her/hers)
Assistant Professor of Pediatrics
University of New Mexico School of Medicine
Albuquerque, New Mexico, United States
Presenting Author(s)
Background: Infants with neonatal opioid withdrawal syndrome (NOWS) are monitored and treated in various hospital care settings, including intensive care unit(ICU) settings (NICU, PICU, intermediate care/specialty care nursery) vs non-ICU settings (newborn nursery/mother-baby unit and pediatric floor). The ESC-NOW study, a multicenter trial, found a decreased length of hospital stay(LOS) and receipt of medication among opioid-exposed infants managed with the Eat, Sleep and Console care approach(ESC) compared to usual care with the Finnegan(UC), but the association between care setting and LOS for infants receiving pharmacologic treatment has yet to be described.
Objective: To assess LOS for infants who receive pharmacologic treatment for NOWS in ICU settings when compared to non-ICU settings.
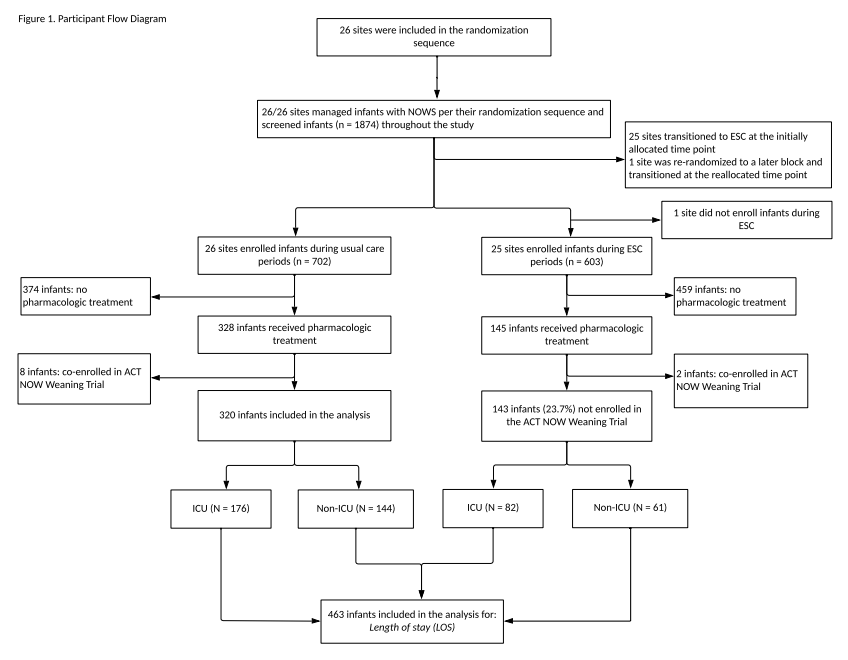
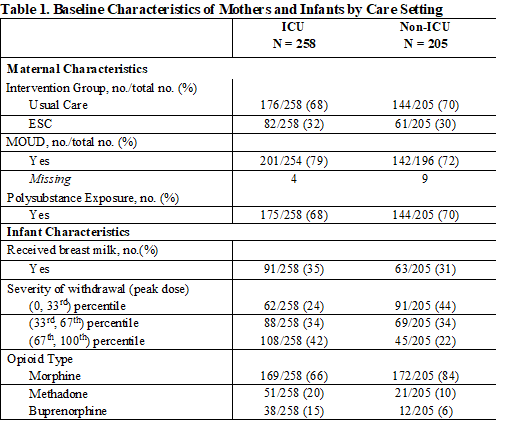
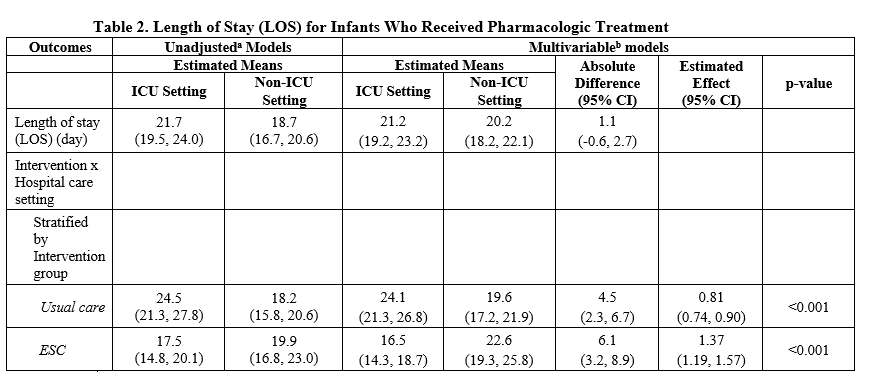
Design/Methods: We studied a cohort of pharmacologically treated infants within ESC-NOW, a stepped-wedge cluster randomized controlled trial. Infants were 36 weeks gestation and treated for NOWS at one of 26 study hospitals. In this analysis, we compared pharmacologically treated infants whose highest level of care was in ICU settings vs non-ICU settings. For LOS we used a generalized linear mixed model with negative binomial distribution and log link function adjusted for study design and maternal and infant characteristics. Following a statistically significant interaction between intervention group (UC vs ESC) and care settings (ICU vs non-ICU), a stratified analysis was conducted by intervention group.
Results: Of 1305 infants enrolled in the ESC-NOW trial, 463 infants received pharmacologic treatment (n=473) and were not co-enrolled in the ACT NOW Weaning Trial. These infants were included in the current analyses. The stratified analysis found that infants managed with UC had a longer LOS in ICU settings than non-ICU settings (24.1 days vs 19.6 days [p < 0.001]) while infants managed with ESC in ICU settings had a 6.1 day shorter mean LOS (16.5 days vs 22.6 days [p < 0.001]) when compared to those in non-ICU settings (n=205[44%]).
Conclusion(s): Results from this secondary analysis showed an increased LOS for infants who were managed with ESC and received pharmacologic treatment in non-ICU settings. This could reflect differences in treatment protocols between care settings or may be resulting from increased opportunities for family involvement and shared decision making in non-ICU settings leading to prolonged weaning of pharmacologic treatment. This represents an area for further exploration as we look to provide care for infants with NOWS in lower acuity environments.