Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 4: Congenital Heart Disease
176 - Effect of Hydrocortisone (HC) on Cardiac Mass in Preterm Intubated Infants < 30 weeks Gestational Age
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 176
Publication Number: 176.2738
Publication Number: 176.2738
- SC
Sanjay Chawla, MD (he/him/his)
Professor of Pediatrics
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Dexamethasone use in preterm infants has been associated with adverse effects including hypertension, and an increase in the left ventricular mass index (LVMI), a surrogate for left ventricular hypertrophy. There are few data on the effects of hydrocortisone (HC) on cardiac mass and function. An increased LVM is a known risk factor for cardiovascular morbidity
Objective: (1) To determine if HC therapy in preterm ventilated neonates is associated with an increase in the LVMI at 36 weeks postmenstrual age (PMA) compared to placebo; (2) to compare the incidence of pulmonary hypertension at 36 weeks PMA in these infants
Design/Methods: Prospective secondary study of a subset of infants in the NICHD Neonatal Research Network RCT, “Hydrocortisone to Improve Survival without Bronchopulmonary Dysplasia” (N Engl J Med 2022:1121). Infants eligible for the RCT were < 30 weeks’ GA without major anomaly, 14-28 days postnatal age, intubated, and had received ≥ 7 days of mechanical ventilation. Infants were randomized to a tapering course of HC from 4mg/kg/day over 10 days or placebo. For this study, a sample size of 124 was needed to detect a 10% difference in the primary outcome (LVMI). Secondary outcomes were pulmonary hypertension, systemic blood pressure, and cardiac wall thickness. This study involved an echocardiogram at 36 weeks PMA, read by a central reader masked to trial intervention. The effect of HC on LVMI was evaluated using linear regression adjusted for the trial stratification factors (center and gestational age strata)
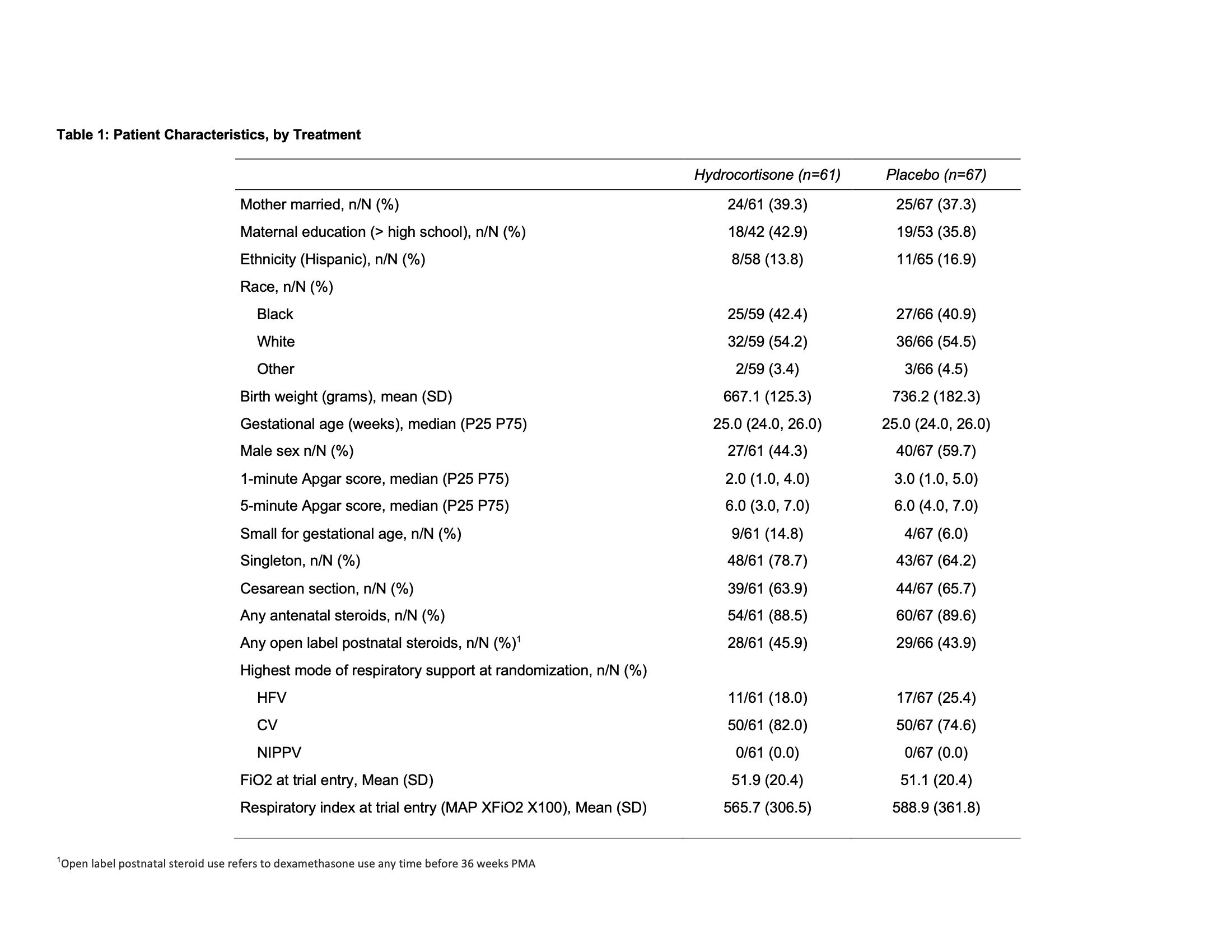
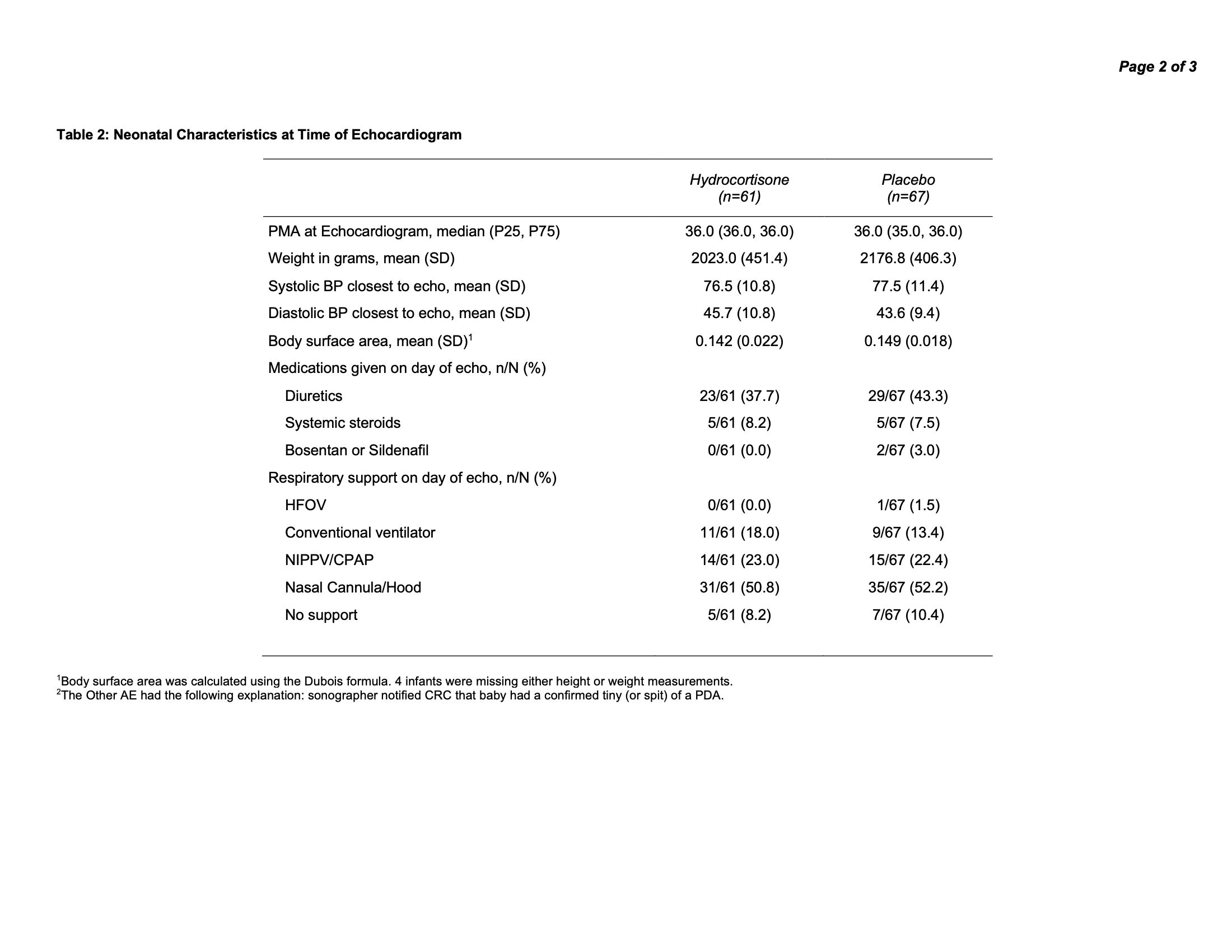
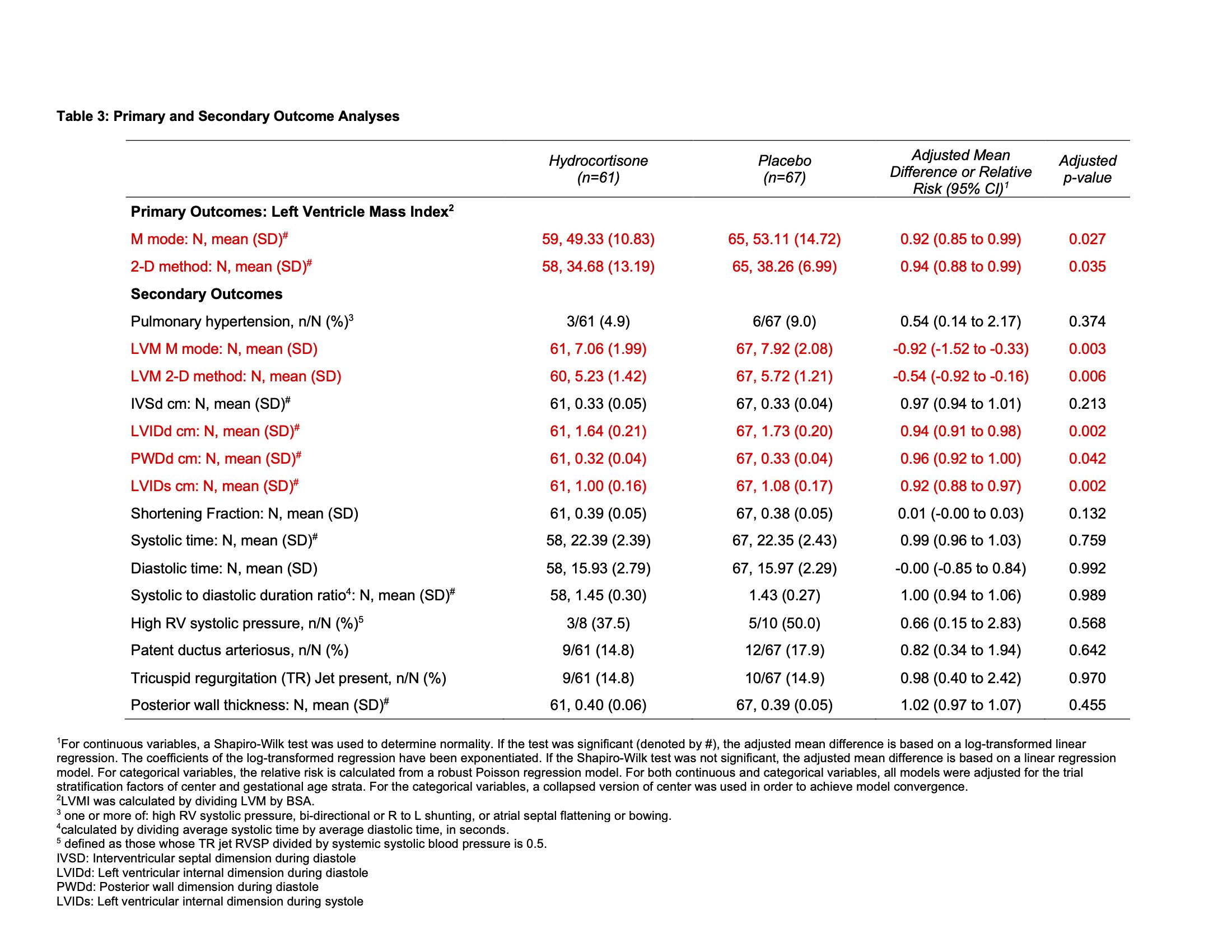
Results: 128 (61 HC, 67 placebo) infants were included. Baseline characteristics at randomization and at time of echocardiogram are in Table 1 and Table 2. The primary outcome, mean LVMI, was lower among patients in HC group, compared to patients in the placebo group (49.3 vs 53.1, p=0.027). The left ventricle internal diameter dimension in diastole and systole and posterior wall thickness were significantly lower among patients in the HC group (Table 3). Pulmonary hypertension was noted in 4.9% of infants in the HC group, compared to 9% in placebo group (p=0.37). None of the infants in the HC group were receiving sildenafil or bosentan at 36 weeks’ PMA, vs 2 (3%) in the placebo group
Conclusion(s): Among extremely preterm infants, a 10-day tapering course of hydrocortisone initiated between 2 and 4 weeks of age was associated with lower LVMI at 36 weeks PMA, compared to placebo. Long term clinical significance of this change should be explored. No significant functional or structural adverse cardiac effects were seen with use of 10 day course of postnatal hydrocortisone