Neonatology
Session: Neonatal Pulmonology - Clinical Science 4: Clinical Practice Questions, Going Home
568 - Pilot Study to Identify Novel Predictors of Extubation or Tracheostomy in Preterm Infants with Grade 3 BPD
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 568
Publication Number: 568.2740
Publication Number: 568.2740
- RG
Ruby Gupta, MD MS (she/her/hers)
Associate Professor
Medical College of Wisconsin
MCW
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Infants with Grade 3 BPD (sBPD) have high risk of need for tracheostomy and long-term ventilation. Despite identified risk factors such as pulmonary hypertension, small for gestational age, postnatal growth failure, and postnatal corticosteroid exposure, there are still unidentified reasons for intercenter variation in tracheostomy use across children’s hospital NICUs.
Objective: To identify candidate variables for potential inclusion to refine future studies of predictors of tracheostomy placement in infants with Grade 3 BPD.
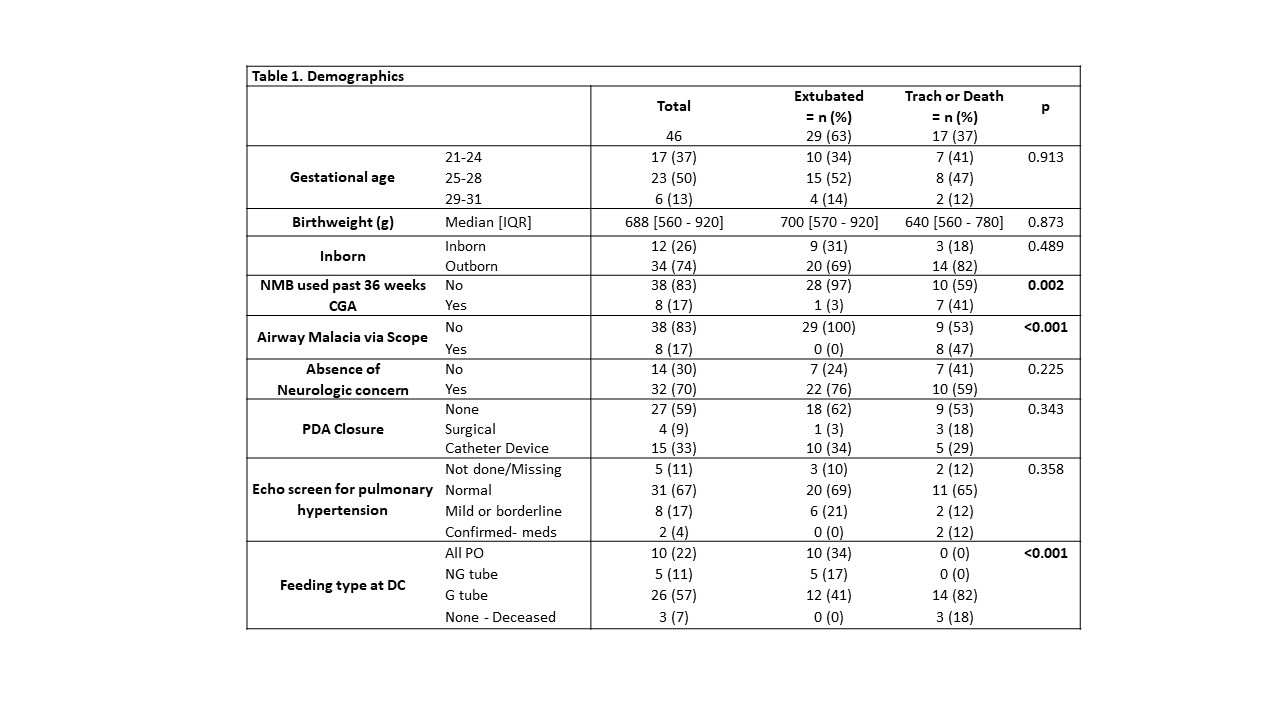
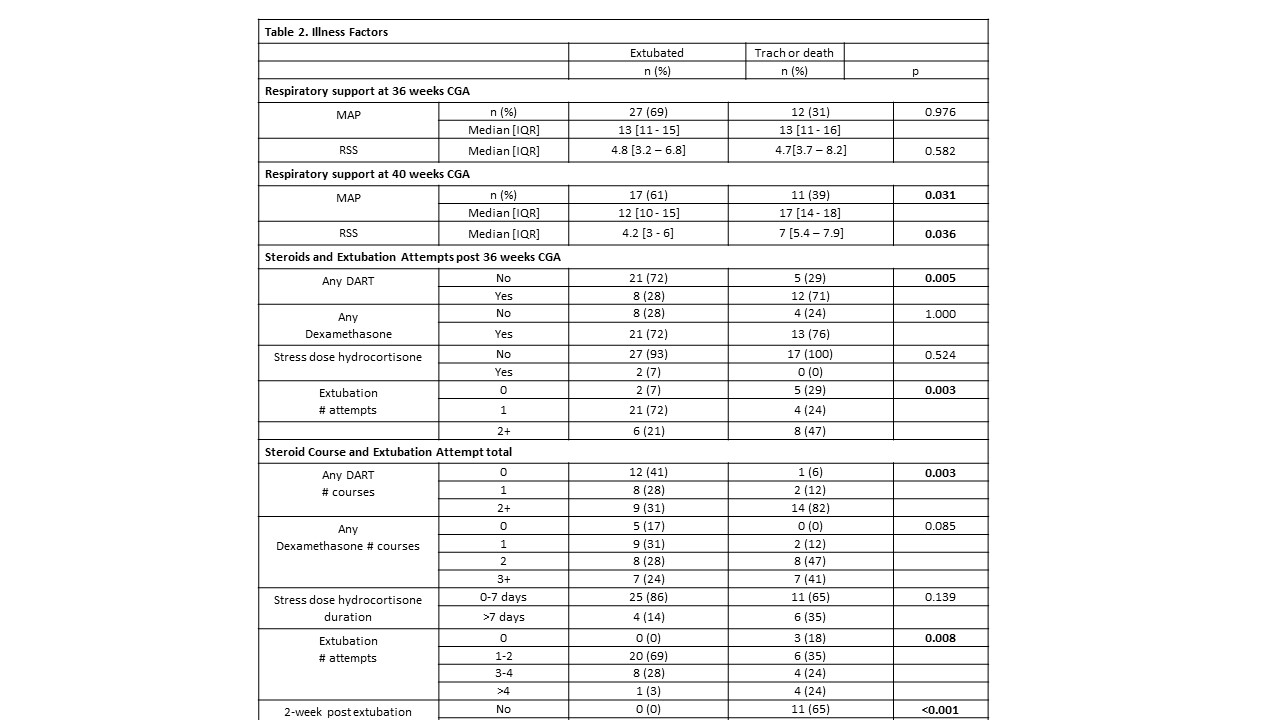
Design/Methods: Single center retrospective chart review of infants with Grade 3 BPD (Mechanical ventilation at 36 weeks corrected age) from 2019-2023, excluding infants with major anomalies. Between 36 weeks and successful extubation or tracheostomy placement, we manually reviewed charts for the following: number of extubation attempts; specific types of postnatal corticosteroid courses; 36 and 40 weeks mean airway pressure, positive end-expiratory pressure, fraction of inhaled oxygen and respiratory severity score (RSS); documented airway malacia by direct visualization; neuromuscular blockade. We compared infants who received tracheostomy to those who extubated. A p-value of < 0.05 was considered significant.
Results: Of 46 patients with sBPD, 37% received tracheostomy (Table 1). There were no differences between groups for gestational age, inborn status, PDA closure, IVH or seizures, or pulmonary hypertension. 47% of infants with tracheostomy were diagnosed with airway malacia, 41% used neuromuscular blockers (NMB) prior to tracheostomy. Compared to patients who extubated, patients receiving tracheostomy had similar MAPs and RSS at 36 weeks cGA but higher MAPs at 40 weeks cGA based on those who were intubated and in our NICU for comparison (Median IQR- 10-15 vs 14-18) and higher RSS (Median IQR- 3-6 vs 5.4-7.9). Patients receiving tracheostomy were more likely to receive >2 courses of DART (82% vs 31%) and have >4 failed extubation attempts (Table 2).
Conclusion(s): In infants with Grade 3 BPD, potential variables identifying risk of tracheostomy placement include MAP and RSS at 40 weeks’ CGA, number of courses of postnatal steroids and extubation attempts, and receipt of neuromuscular blockade. These variables may be useful in future research and quality improvement initiatives to improve care for this high-risk patient population.