Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 2
376 - Improving Patient-Centered Continuity of Care in a Pediatric Primary Care Resident-led Clinic: A Quality Improvement Initiative
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 376
Publication Number: 376.2085
Publication Number: 376.2085

Liz Yovanna Bayes, MD MS
Associate Professor of Pediatrics
University of Miami
Miami, Florida, United States
Presenting Author(s)
Background: Continuity of care, the ongoing medical relationship between physician and patient, plays a critical role in primary care residency teaching clinics. However, it can be challenging to establish due to residents’ competing clinical responsibilities. Continuity of care is a driver of patient and physician satisfaction associated with better patient health outcomes.
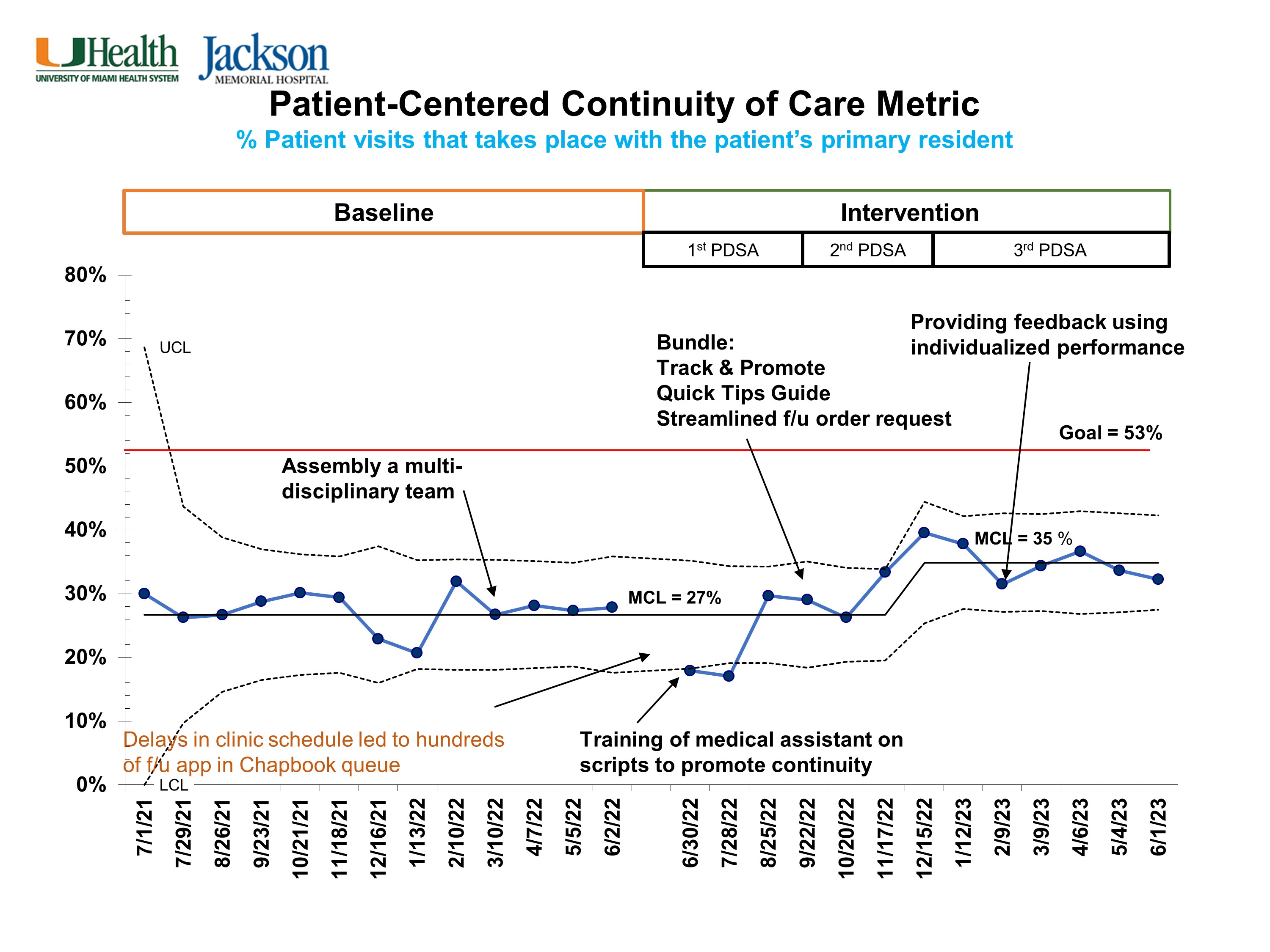
Objective: We aimed to improve patient-centered continuity of care (P-CCC) rates in our pediatric resident-led clinics from a baseline of 27% to greater than the national median of 53% by June 2024.
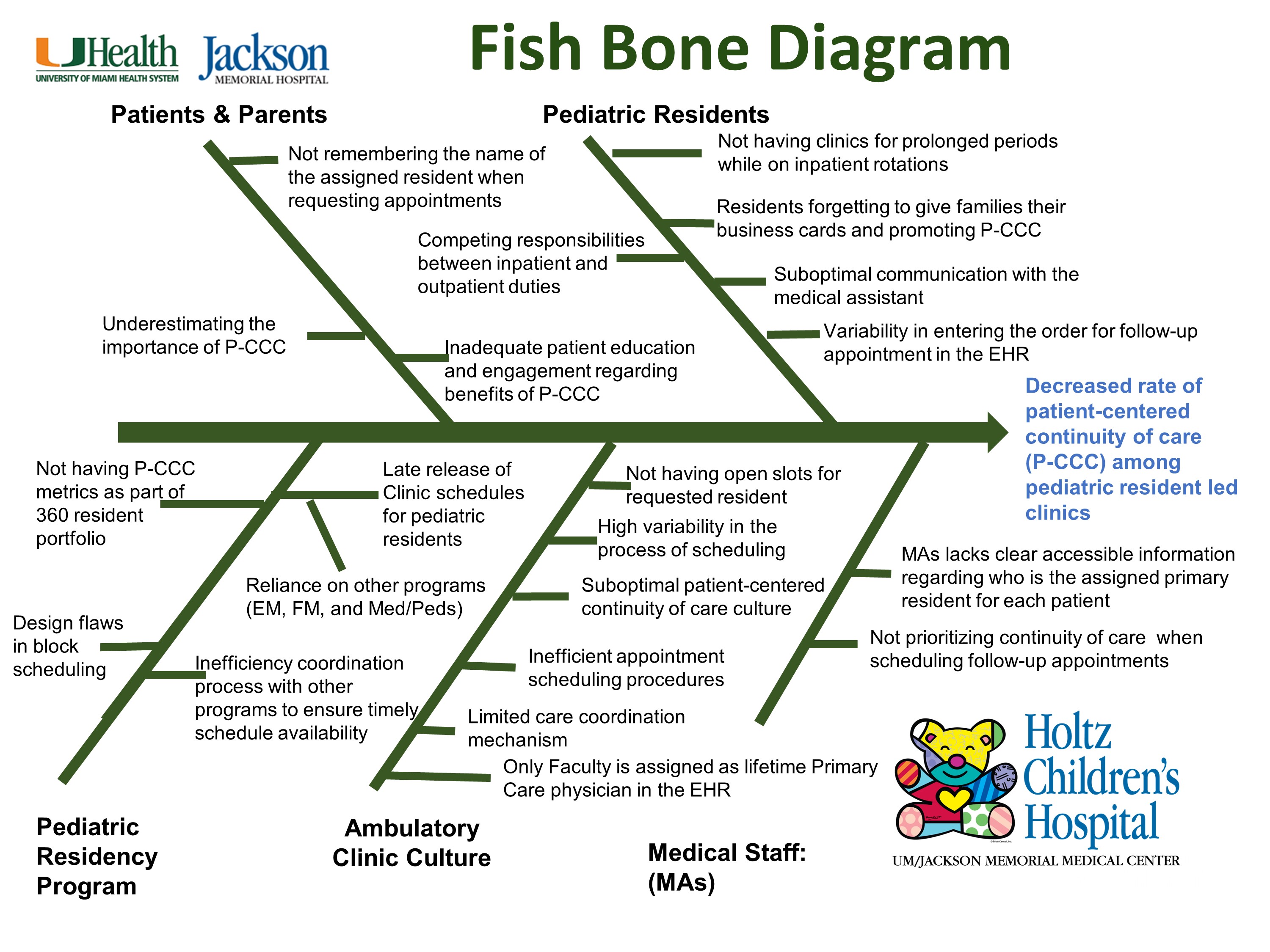
Design/Methods: A multidisciplinary team formed in March 2022 reviewed the process of scheduling follow-up appointments. Root cause analysis identified contributing factors to low P-CCC rates (Figure 1). Barriers to P-CCC were: difficulty among staff to determine a patient’s primary resident, poor communication between clinic staff and residents, high variability in the process of scheduling follow-up appointments, lack of same day appointments for sick visits, and late release of residents’ clinic schedules. We developed a key driver diagram to plan our interventions, which included: resident buy-in, faculty engagement, a standardized scheduling process, adoption of strong continuity culture, enhanced communication among residents and clinic staff, and providing individualized P-CCC performance (Figure 2). We conducted Plan-Do-Study-Act (PDSA) cycles then enacted interventions theorized to have the most impact on our drivers. The primary outcome was the monthly P-CCC rate defined as patients seen by the primary resident divided by the total number of patients seen in the clinic with at least 2 clinical encounters in the dataset. A statistical process control chart was used to display data overtime.
Results: This is an ongoing initiative. A total of 9586 clinical encounters from 3105 patients were analyzed from July 2021 to June 2023. During the study period, P-CCC improved from 27% to 35%, a 30% increase (Figure 3). We observed special cause variation in November 2022 after standardization of follow-up appointment scheduling and providing residents with a printout of strategies to improve P-CCC during the second PDSA cycle. This improvement was sustained after the third PDSA cycle.
Conclusion(s): P-CCC rates in the pediatric resident-led clinic improved by 30% via implementation of data-driven interventions. We anticipate a continued upward trend in subsequent PDSA cycles including a new scheduling algorithm, increased appointment slots, and use of the electronic medical record to clearly identify a patient’s primary resident.
.jpg)