Neonatology
Session: Neonatal Neurology 2: Clinical
28 - Relationship between severity of clinical encephalopathy and EEG background in neonates with hypoxic-ischemic encephalopathy treated with therapeutic hypothermia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 28
Publication Number: 28.443
Publication Number: 28.443
- MC
Marie C. Cornet, MD PhD (she/her/hers)
Assistant Professor
University of California San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: Treatment with therapeutic hypothermia (TH) improves neurodevelopmental outcomes in neonates with moderate and severe hypoxic-ischemic encephalopathy (HIE). Assessing eligibility for TH in the first hours of life is challenging. The EEG background quantifies brain dysfunction. Some centers rely on clinical encephalopathy alone, while others also require an abnormal EEG. Yet, the association between the severity of clinical encephalopathy assessed by a modified Sarnat exam and EEG dysfunction assessed by clinical EEG reads is seldom described.
Objective: To assess the association between the severity of clinical encephalopathy and severity of brain dysfunction by EEG on the first day of life (DOL1).
Design/Methods: Infants enrolled in the High-dose Erythropoietin for Asphyxia and Encephalopathy (HEAL) trial with EEG or aEEG report available on DOL1 were included. EEG background continuity was categorized as normal, excessively discontinuous, or severely abnormal based on EEG reports. The severity of clinical encephalopathy was assessed by Sarnat exam performed by trained investigators on DOL1. We assessed the association between severity of clinical encephalopathy and EEG background using descriptive statistics and proportional odds regression.
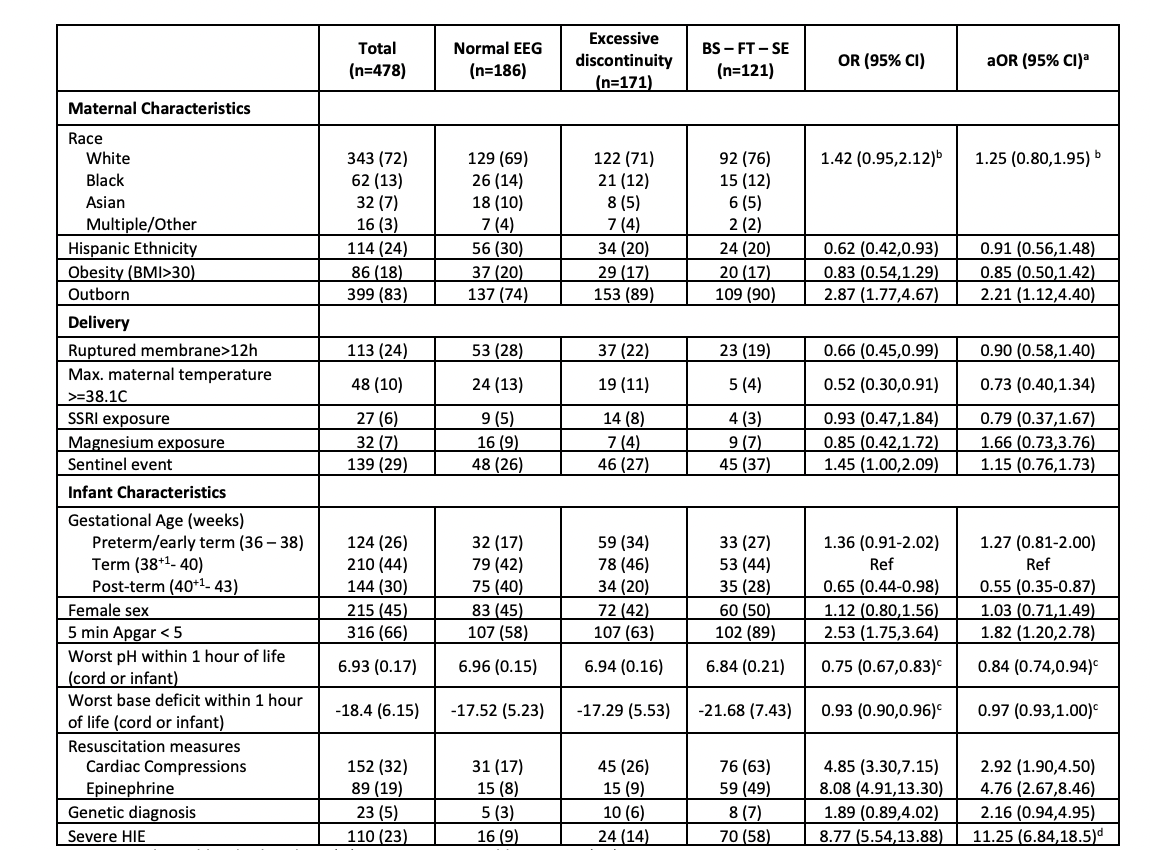
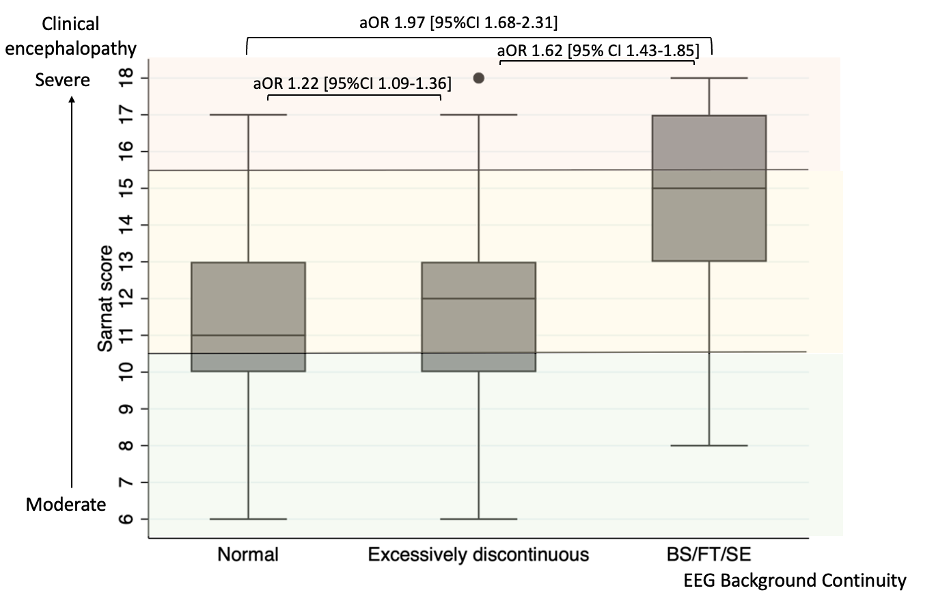
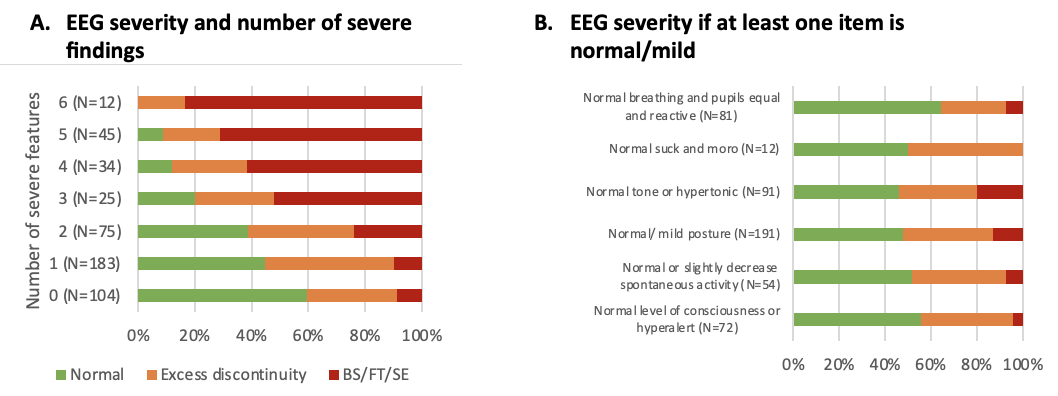
Results: Among 500 infants in the HEAL trial, 478 (96%) had interpretable EEG reports. The EEG background was normal in 186 (39%), excessively discontinuous in 171 (36%), and severely abnormal in 121 (25%). EEG background severity was associated with birth location, gestational age, Apgar score, resuscitation at birth, and acidosis (Table 1). There was a significant association between Sarnat score and EEG severity (Figure 1) or number of severe findings on exam (Figure 2A). Infants who scored normal or mild in at least one category had >50% chance of having a normal EEG (Figure 2B). Some infants had discordant exam and EEG findings. Among infants with milder encephalopathy ( < 2 severe exam findings), the ones with a severe EEG had lower Apgar scores (p=0.002) and more sentinel events (RR 2.3 [95%CI 1.2-4.6]) compared to those with more severe clinical encephalopathy.
Conclusion(s): In this cohort, more than a third of infants with moderate or severe clinical encephalopathy had a normal EEG background. While the clinical severity of encephalopathy and EEG background abnormalities are closely associated, they are not entirely correlated. Further studies are needed to determine which is better for predicting outcomes and whether infants with a normal EEG background do benefit from cooling.