Developmental and Behavioral Pediatrics
Session: Developmental and Behavioral Pediatrics 4: Potpourri
602 - Individual and Relational Correlates of Adolescent Socioemotional Health
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 602
Publication Number: 602.2224
Publication Number: 602.2224
- MH
Marie Heffernan, PhD (she/her/hers)
Assistant Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Adolescent socioemotional health is multifaceted and includes individual components such as stress and well-being, as well as relational components such as relationship quality and satisfaction. Socioemotional health in adolescence also is associated with health across the life course.
Objective: The goals of this project were to identify individual and relational factors associated with adolescent socioemotional health.
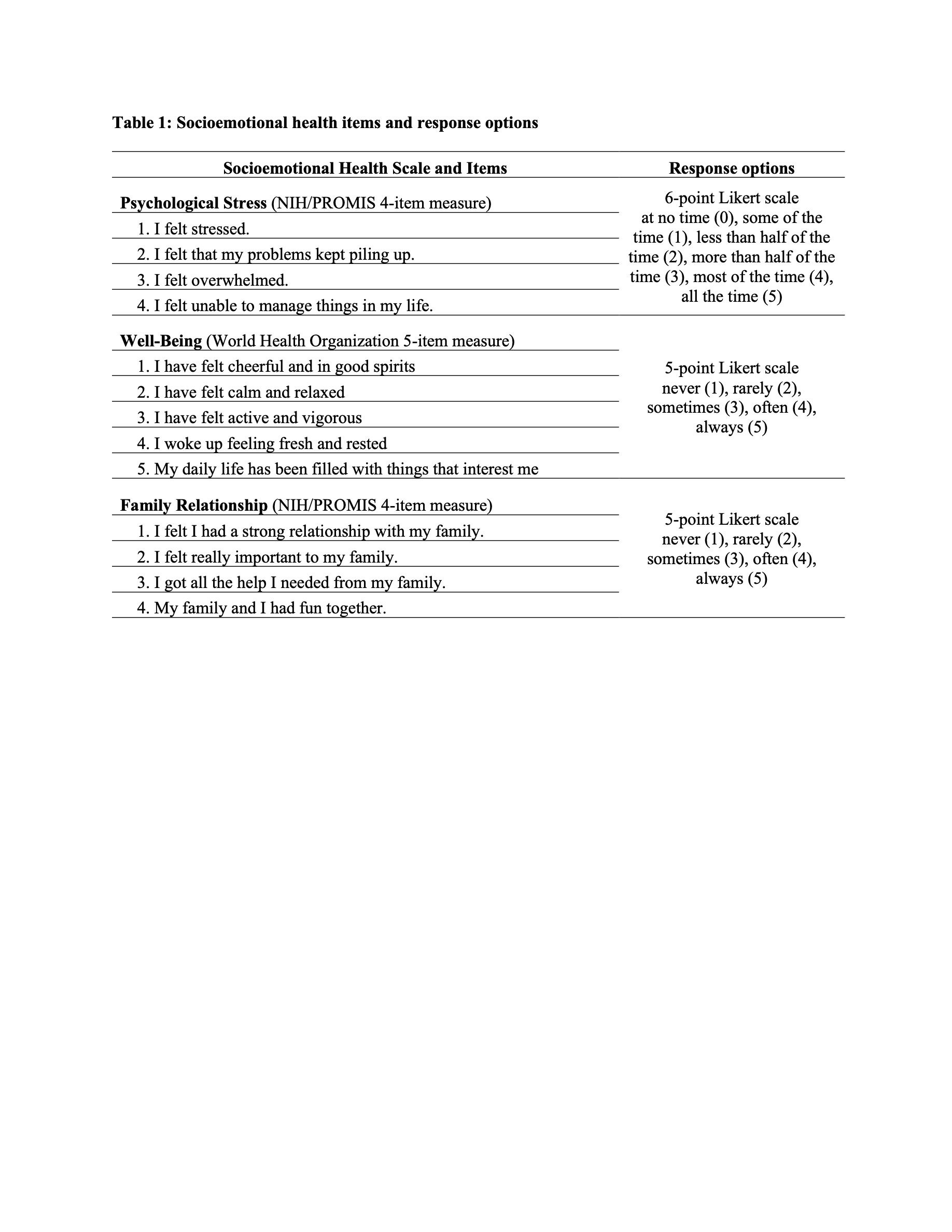
Design/Methods: Data were collected from November 2021-February 2022. Parents completed a survey via web or phone through the Voices of Child Health in Chicago Parent Panel. Parents were eligible if they had at least one child 12-17 years old. Adolescents completed a web-based survey via Qualtrics. Respondents self-reported their demographics. This study focuses on parent and adolescent responses on the adolescent’s psychological stress, well-being, and family relationship (Table 1). Adolescents also completed scales on relational (e.g., attachment) and individual (e.g., personality) factors. We conducted three multiple regression models, one for each adolescent socioemotional health variable, and included relational and individual predictor variables. We assessed for multicollinearity among predictor variables.
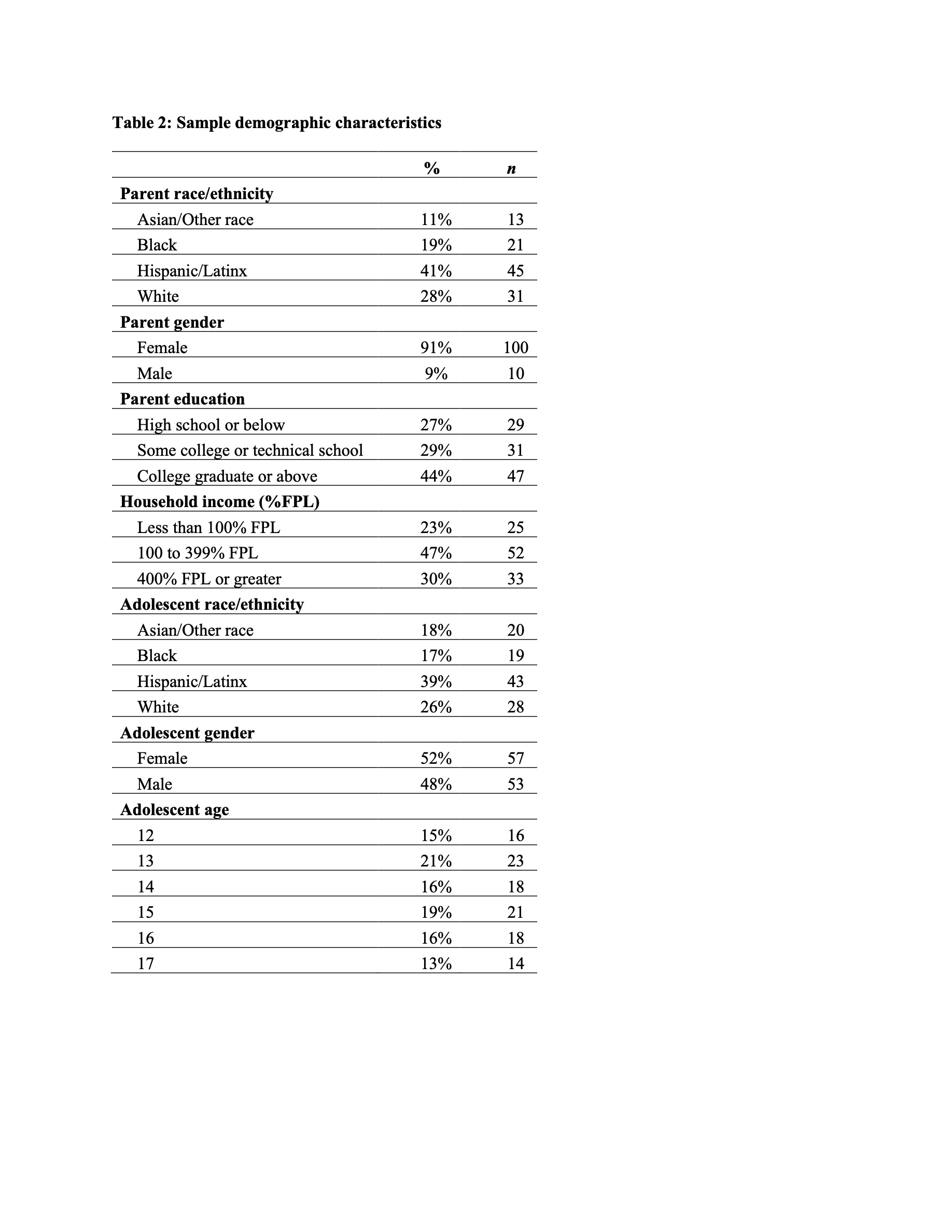
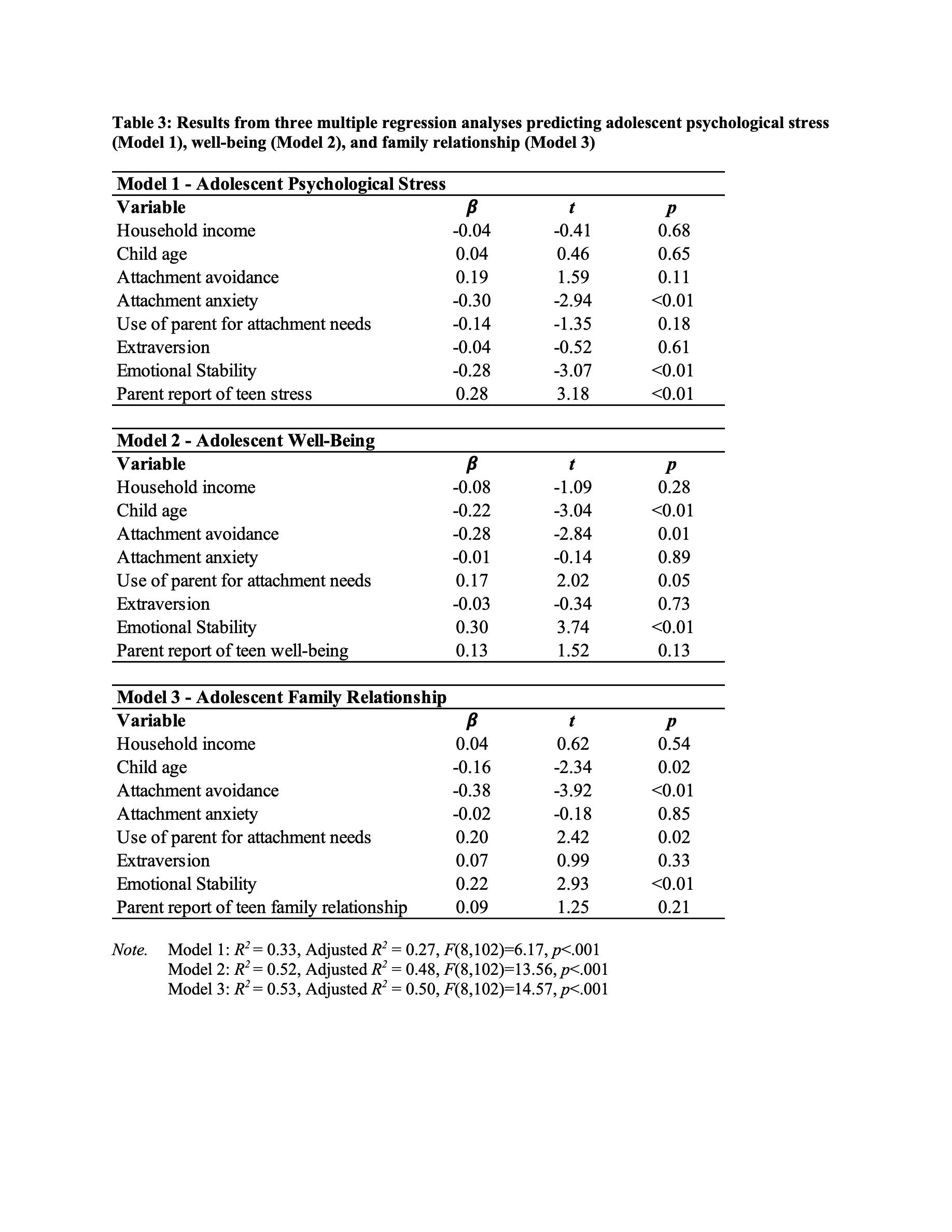
Results: Responses were obtained from 111 parent-child dyads (Table 2). The overall survey completion rate was 34.4% for parents and 64.5% for adolescents. Multivariable analyses revealed that for adolescent psychological stress, higher attachment anxiety (worry about relationships) was associated with lower stress (Table 3, Model 1), as was higher emotional stability. Parent ratings of their child’s psychological stress also significantly predicted adolescents’ self-ratings of psychological stress. For adolescent well-being, children with more avoidant attachment (discomfort with emotional closeness) had worse well-being scores, as did older children overall; higher emotional stability was associated with higher well-being scores (Table 3, Model 2). For family relationship, higher attachment avoidance was associated with lower family relationship scores, whereas using the parent for attachment/emotional needs and emotional stability were associated with better family relationships (Table 3, Model 3).
Conclusion(s): Emotional stability was consistently associated with better socioemotional health for adolescents, and attachment avoidance was consistently associated with worse socioemotional health for adolescents. It may be helpful to administer these brief instruments in primary care settings, given the strong association of socioemotional wellness with health overall.