Neonatology
Session: Neonatal-Perinatal Health Care Delivery: Practices and Procedures 3
478 - Anthropometric Measurements and Incidence of Respiratory Infections After Delayed Cord Clamping in Term Neonates
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 478
Publication Number: 478.2807
Publication Number: 478.2807
- RG
Ronique C. Gordon, M.B.B.S. (she/her/hers)
Pediatric Resident
Flushing Hospital Medical Center
Flushing, New York, United States
Presenting Author(s)
Background: Delayed cord clamping (DCC) refers to passive transfer of blood from mother to newborn for >30 seconds before clamping and cutting the umbilical cord. The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics recommend DCC for at least 30-60 seconds for most vigorous term babies. There are no studies comparing postnatal growth and immunologic outcomes in term infants receiving DCC.
Objective: To determine if DCC improves growth and reduces incidence of RI in term newborns.
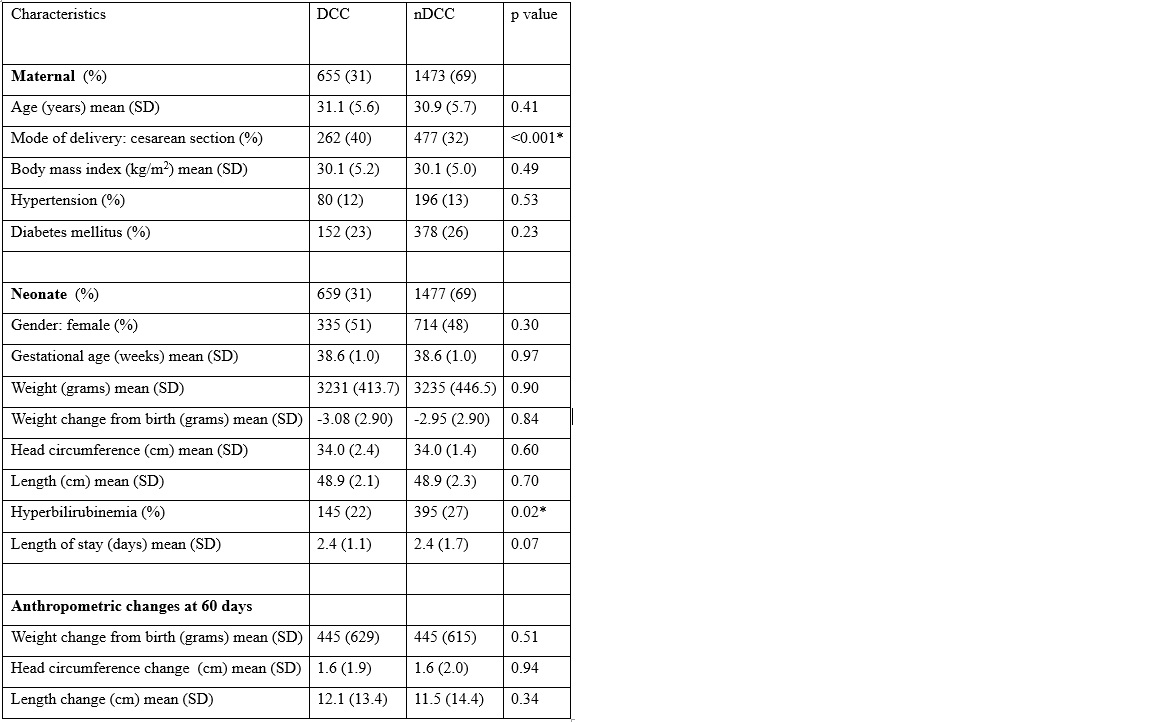
Design/Methods: Retrospective chart review of term newborns born at an urban community hospital between Jan 1, 2022 and Dec 31, 2022 who either had DCC or did not have DCC (nDCC) for 30-60 seconds at birth. Data extracted from the mother’s medical record included age, mode of delivery, body mass index (BMI), hypertension and diabetes mellitus. Neonatal data included gender, gestational age, anthropometric measurements, hyperbilirubinemia, length of stay (LOS), number of emergency department (ED) visits and hospital admission for respiratory infections (RI) at 60, 90 and 180 days post initial discharge. Data were analyzed with Pearson correlation coefficient, chi-square and Wilcoxon rank-sum tests, p< 0.05 was considered significant.
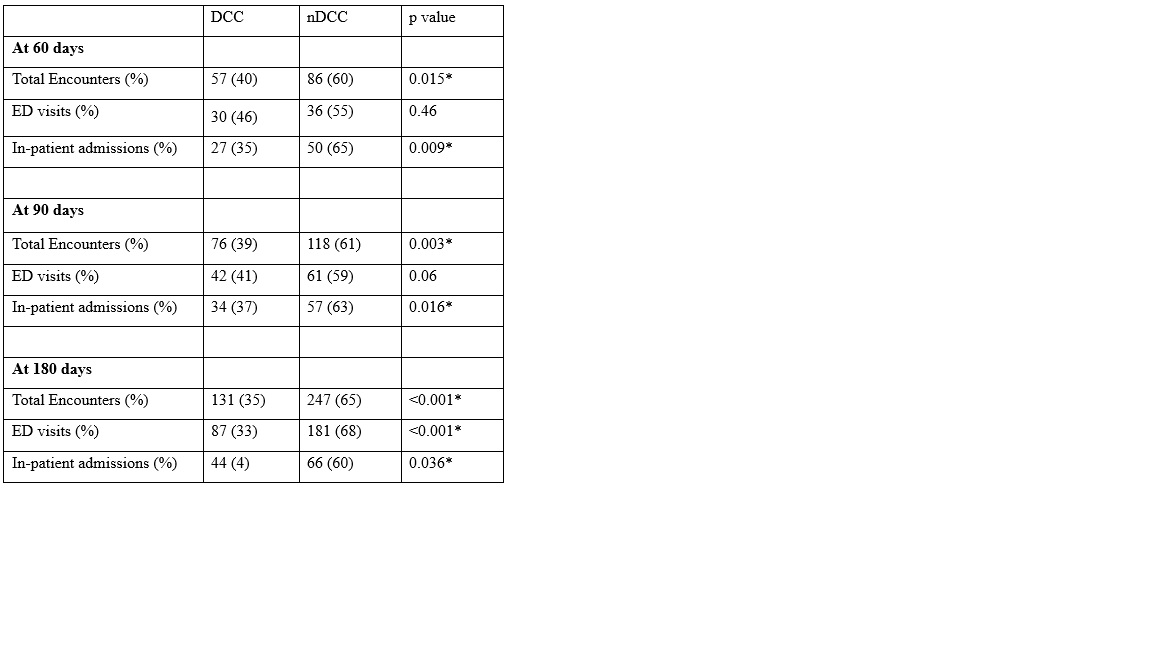
Results: Of 2,136 charts reviewed, 1,477 (69%) were in nDCC group and 659 (31%) in DCC group. When comparing the two groups, there was no significant difference in maternal age, BMI, hypertension and diabetes mellitus, neonate gender, gestation age, anthropometric measurements and LOS, p>0.05. The rate of cesarean section was 35%, higher in the DCC group (40%) compared to nDCC group (32%), p< 0.001. For the neonate, the rate of hyperbilirubinemia was significantly higher in nDCC (27%) group compared to DCC (22%) group, p=0.02, table 1. At 60 days post-discharge, more patient encounters for RI were in nDCC group (60%) compared to DCC (40%), p=0.015. This trend continued at 90 days (p=0.003) and at 180 days (p < 0.001). The higher rate of inpatient RI related admissions at 60, 90, and 180 days post-initial discharge was also significant, p< 0.01, table 2.
Conclusion(s): In our sample, a higher rate of cesarean section was in those who received DCC. There was no increased risk of hyperbilirubinemia in the DCC group. No differences were found in anthropometric measurements in both groups. DCC was associated with lower number of ED visits and in-patient admissions for acute RI in the first 180 days of life.