Breastfeeding/Human Milk
Session: Breastfeeding/Human Milk 2: Human Milk Feeding
491 - Disparities in exclusive breast milk feeding among infants discharged from an academic medical center: the role of language barriers and donor milk
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 491
Publication Number: 491.2262
Publication Number: 491.2262

Temitope Awelewa, MBCHB, MPH, IBCLC, NABBLM-C
Clinical Associate Professor
University of Iowa
Iowa City, Iowa, United States
Presenting Author(s)
Background: The American Academy of Pediatrics (AAP) recommends exclusive breast milk (EBM) feeding for 6 months to reduce maternal and infant mortality. Unfortunately, there are significant disparities in EBM feeding among racial groups. Our team recently facilitated an AAP Community Access to Child Health-sponsored focus group that included recent immigrants from the Democratic Republic of Congo and Togo. Most of the participants breastfed less than they intended. They indicated communication issues contributed to a lack of knowledge about the benefits of EBM feeding and the use of donor milk.
Objective: Explore the influence of sociodemographic factors in EBM feeding and the utilization of donor milk at discharge from the University of Iowa Stead Family Children’s Hospital (SFCH)
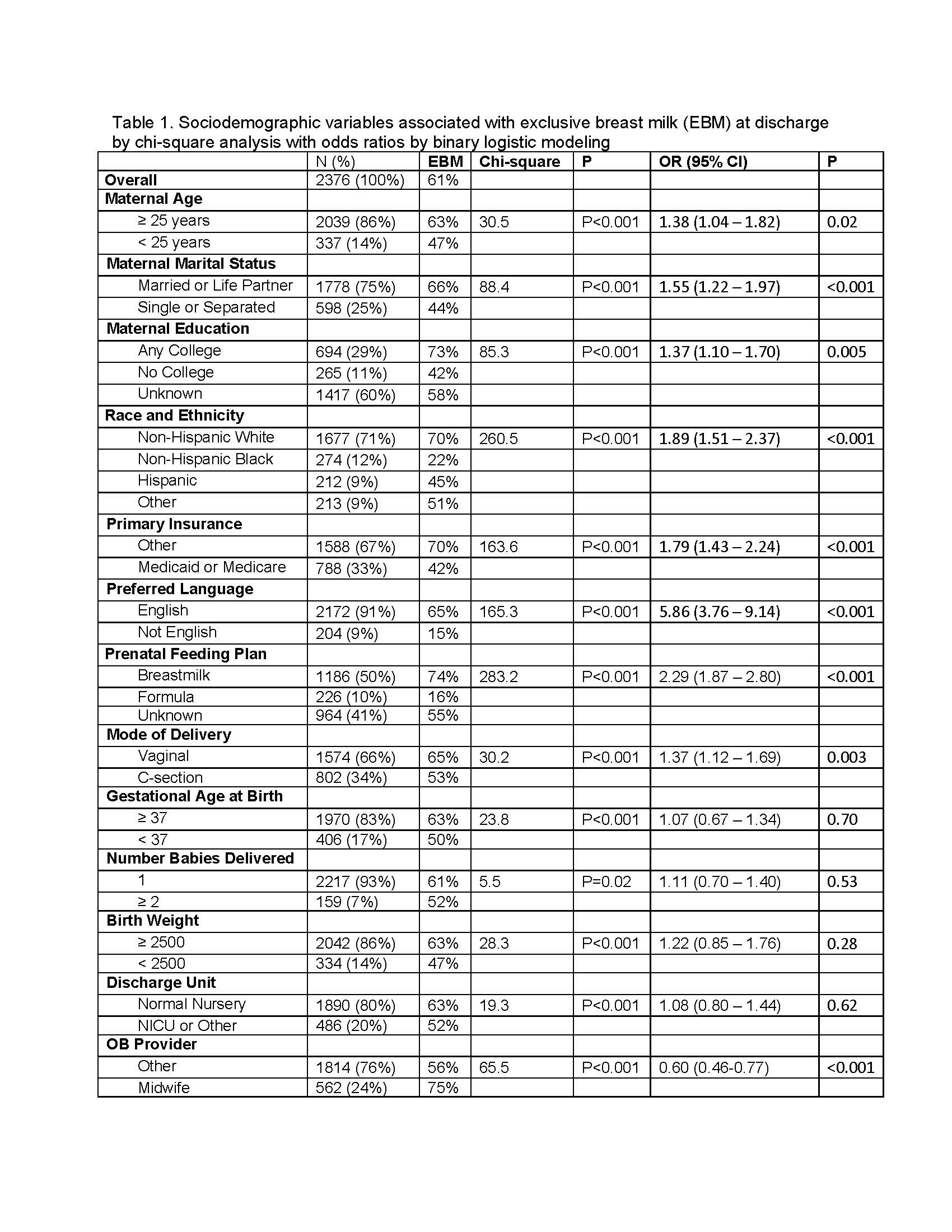
Design/Methods: Following IRB approval, we reviewed electronic medical records (EMR) of all infants born at the SFCH and discharged between January 1, 2023 and September 30, 2023. Independent variables were identified by multidisciplinary taskforce recommendations. Dependent variables included EMR-documented receipt of maternal milk, donor milk, or formula. Chi-square analysis and logistic regression were utilized to assess statistical significance.
Results: Of 2376 discharges, the overall EBM rate was 61%. By forward stepwise regression, nine maternal sociodemographic variables predicted EBM (Table 1, P< 0.05), including, in order of entry to the model: race or ethnicity, prenatal feeding plan, insurance coverage, age, preferred language, marital status, prenatal care provider, mode of delivery and educational level. The rate of EBM was lowest for infants whose mothers had non-English language preferences (NELP), and their EBM rate (15%) was even lower than those whose mothers had a prenatal plan to use formula (16% EBM). Of those with NELP, only 35% had a prenatal plan for EBM (versus 51% of those without NELP, P< 0.0001), and only 23% of that subset achieved their desire for EBM feeding (versus 77% of those without NELP, P< 0.0001). Overall, 53% of infants discharged from the NICU received donor milk, including 52% of those whose mother had NELP. EBM feeding was independent of donor milk use for NICU infants, including those with NELP.
Conclusion(s): NELP is an independent risk factor of formula supplementation during an infant’s initial hospitalization. The findings will inform the development and improvement of culturally responsive lactation practices in the health system. Ongoing community outreach with culturally competent maternal education are needed to increase EBM rates and reduce disparities.