Neonatology
Session: Neonatal Pulmonology - Clinical Science 2: Lung Imaging, Lung Function
211 - Pulmonary Function Using Non-Invasive Forced Oscillometry among Infants With and Without Lung Disease (PUFFOR Study)
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 211
Publication Number: 211.2829
Publication Number: 211.2829

Colm P. Travers, MD (he/him/his)
Assistant Professor
University of Alabama School of Medicine
Birmingham, Alabama, United States
Presenting Author(s)
Background: Impulse oscillometry (iOS) is a non-invasive method to assess lung disease severity. Differences in pulmonary mechanics between infants with and without lung disease may persist until discharge, and iOS may objectively measure the nature and magnitude of these differences.
Objective: To test the hypothesis that pulmonary mechanics are worse in preterm infants without RDS vs healthy term-late preterm infants, in preterm infants with RDS vs without RDS, and in preterm infants with BPD vs without BPD.
Design/Methods: Single center prospective observational cohort study enrolling preterm infants 22-34 weeks’ gestation with and without lung disease admitted to the neonatal intensive care unit and healthy term-late preterm infants ≥ 35 weeks’ gestation without lung disease admitted to the newborn nursery. After obtaining informed consent we enrolled infants once not actively receiving positive pressure respiratory support. We measured pulmonary mechanics using FOT at discharge or 40 weeks’ PMA, using the tremoflo N-100 Airwave Oscillometry device (Thorasys, Montreal). Two sets of tests including ≥3 measurements using coefficient of variation < 20% within a 15% agreement threshold were obtained in the supine neutral head position. The primary analysis compared differences in the mean area under the reactance curve (AX). Secondary analyses compared difference in Resistance at 7 Hz (R7), the difference between R7 and resistance at 19Hz (R7-19), and reactance at 7Hz (X7). Data were analyzed using logistic regression adjusted for weight at testing, and sex.
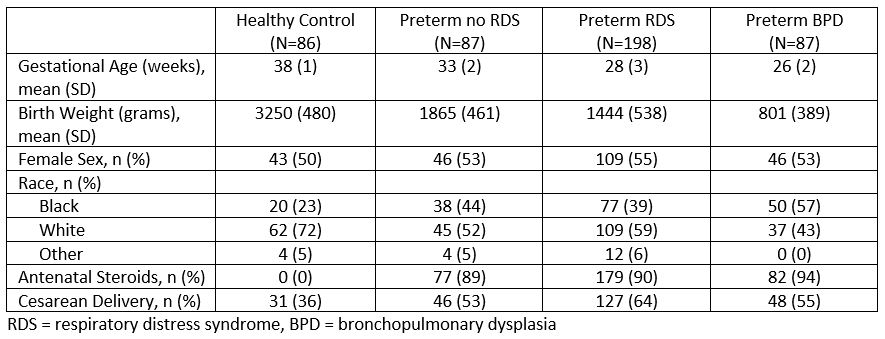
Results: We included 458 infants including 198 with RDS but no BPD, 87 with BPD, 87 preterm without lung disease, and 86 controls. The mean (SD) gestational age was 31 (5) weeks and birth weight was 1729 (935) grams (Table 1). Preterm infants without lung disease had a higher AX compared with term-late preterm infants without lung disease (Table 2). AX differed among preterm infants with RDS and no BPD and preterm infants without RDS/BPD. The AX was higher among preterm infants with BPD compared with preterm infants with RDS but no BPD, but the difference was not statistically significant. The R7-19 was significantly higher among infants with BPD compared to those with RDS but no BPD. Overall, AX decreased with increasing gestational age but differed by BPD status (Figure 1).
Conclusion(s): Abnormal lung mechanics in preterm infants with and without lung disease persist until discharge and are characterized by increased reactance and increased resistance in peripheral airways. Oscillometry may provide an objective measure of lung disease severity in neonates.
.jpg)
.jpg)
