Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 1: PDA
87 - Clinical impact of achieving complete closure of patent ductus arteriosus following primary medical therapy in extremely low gestational age neonates
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 87
Publication Number: 87.2133
Publication Number: 87.2133

Jejelola Ladele, MBChB, FMCPaed
Staff Neonatologist, Assistant Professor
University of Toronto Temerty Faculty of Medicine
Toronto, Ontario, Canada
Presenting Author(s)
Background: Patent ductus arteriosus (PDA) is associated with adverse outcomes in extremely low gestational age neonates (ELGAN); however, its treatment is much debated. It is not clear whether outcomes are related to high failure rate of current primary treatments, resulting in prolonged shunt exposure or preexisting patient characteristics not modifiable by shunt elimination.
Objective: To investigate the relationship between complete shunt elimination and clinical outcomes after first medical therapy for PDA in ELGANs.
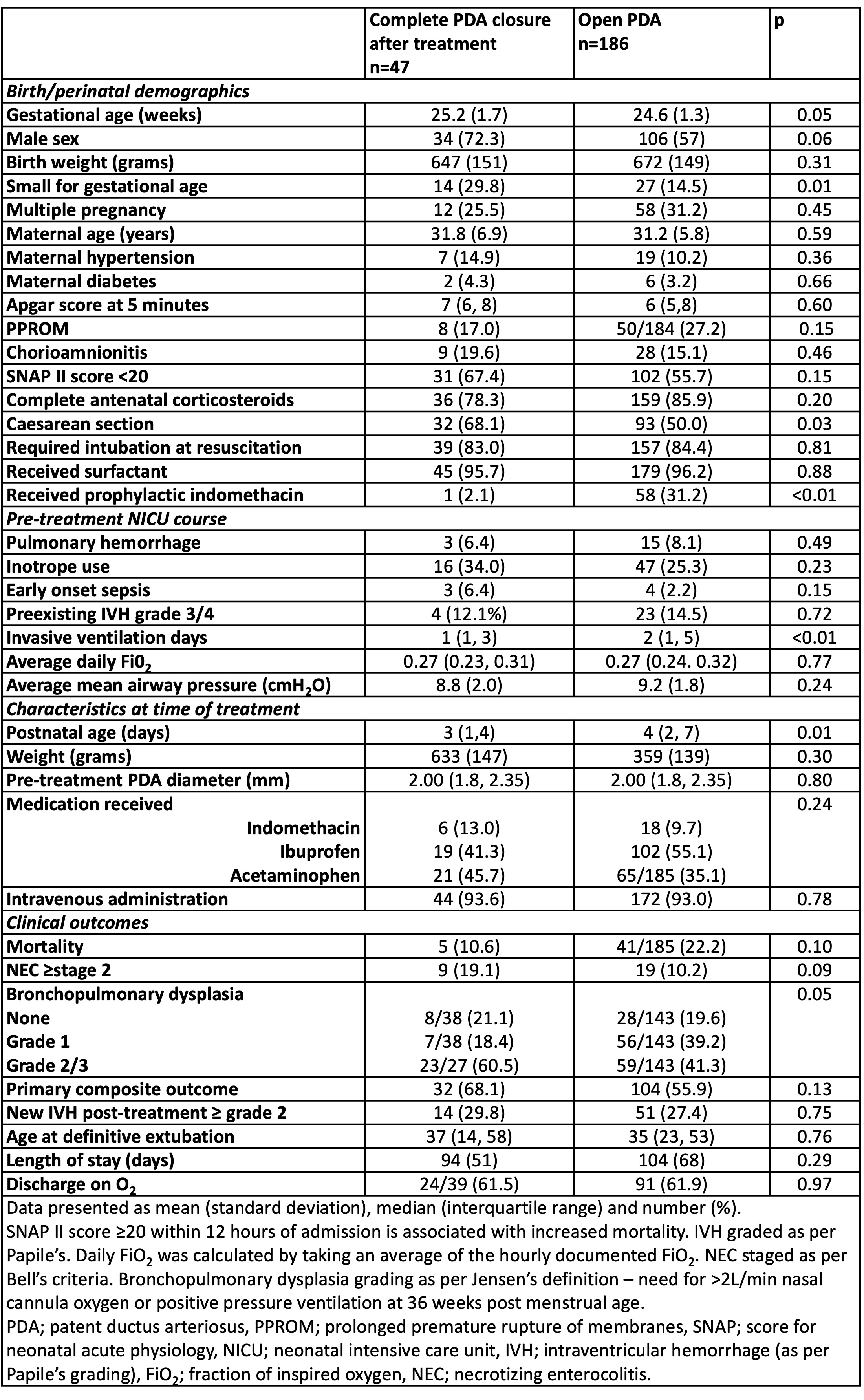
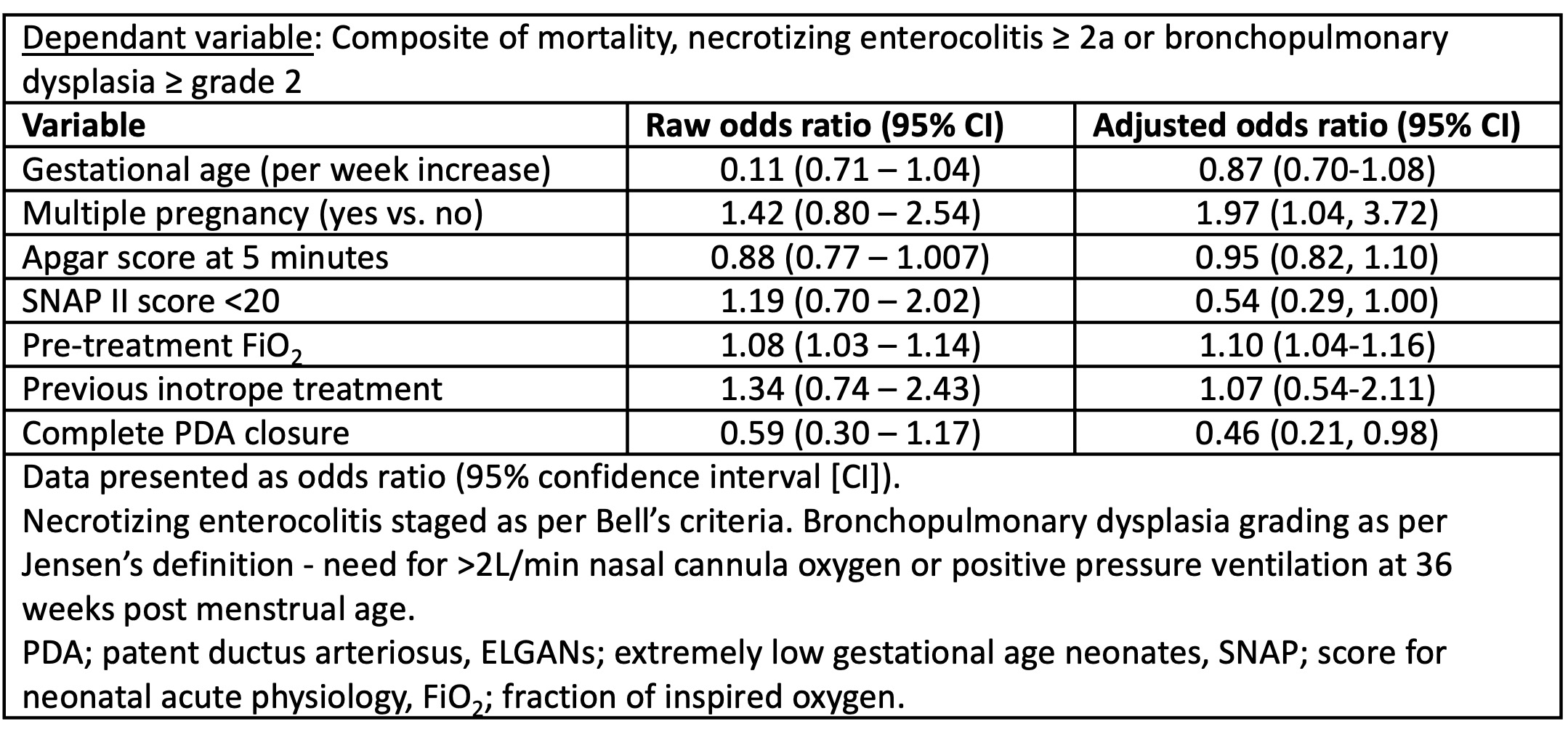
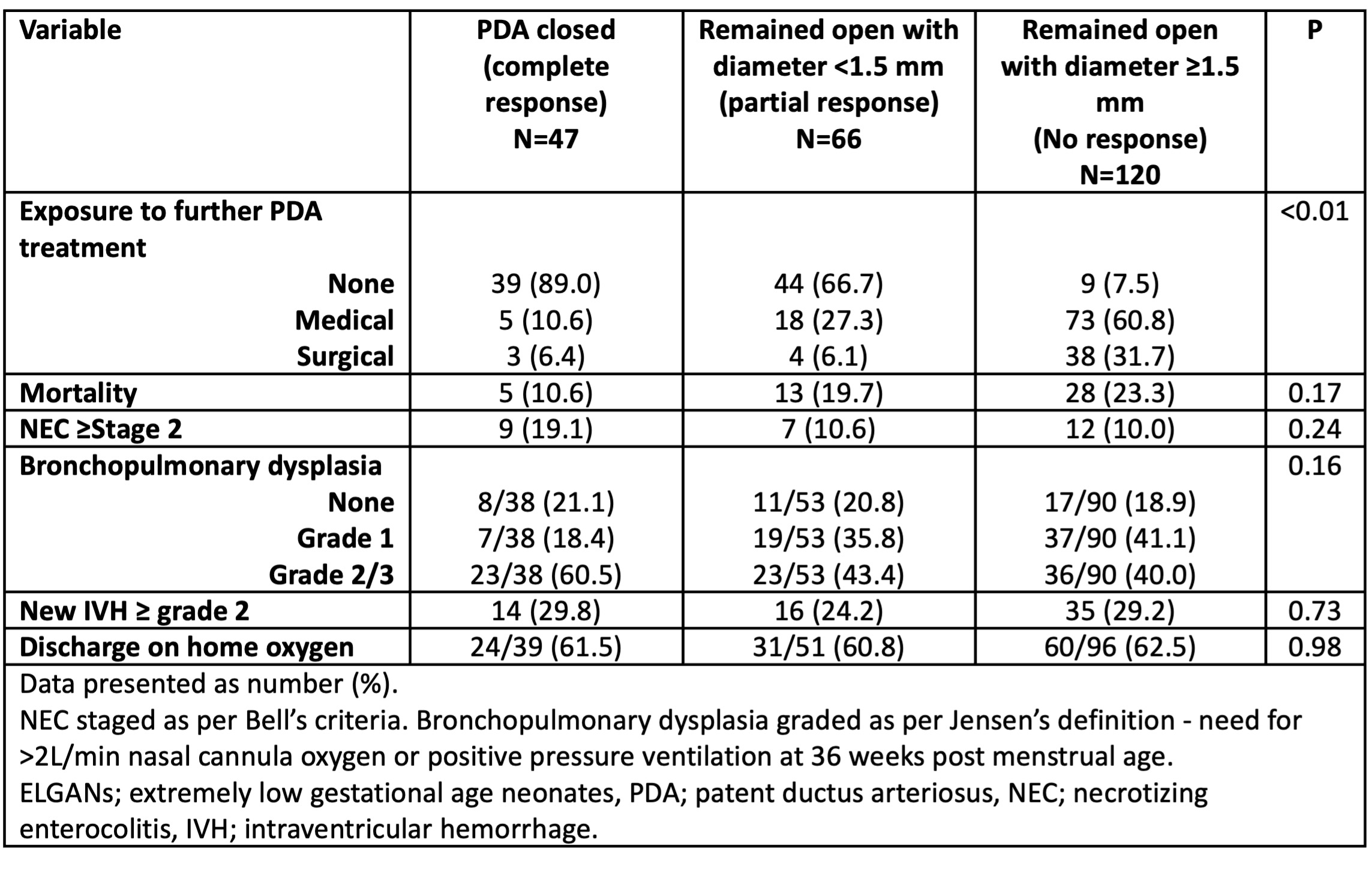
Design/Methods: A retrospective cohort study enrolled neonates with GA ≤27 weeks or birth weight (BW) < 750 grams across 3 tertiary NICUs, who received medical therapy for PDA ≥1.5 mm within 10 days of age. Pre-treatment illness severity data extracted included demographics, mean airway pressure and fraction of inspired oxygen (FiO2) averaged over 24h, days of invasive mechanical ventilation and inotropes. Patients with complete PDA closure were compared to those with persistent shunt after treatment. Primary outcome was composite of mortality, necrotizing enterocolitis (NEC) ≥2a and bronchopulmonary dysplasia (BPD) ≥grade 2 (needing >2L/min nasal cannula oxygen or positive pressure support at 36 weeks postmenstrual age). Logistic regression (LR) analysis was conducted to examine the relationship between shunt elimination and primary outcome, adjusting for predefined confounders. Clinical outcomes were also described in relation to 3 post-treatment PDA status categories: closure, partial closure (diameter < 1.5mm), no response (diameter ≥1.5mm).
Results: The study included 233 infants [mean (SD) GA 24.7 (1.4) weeks, BW 667 (149) grams, and median (IQR) age at treatment 4 (2, 7) days and PDA diameter 2.0 (1.8, 2.3) mm]. Only 47 (20%) had complete PDA closure after treatment; 66 (29%) had partial closure. Complete closure was associated with higher GA, small for GA, less prophylactic indomethacin, and a nonsignificant reduction in mortality (Table 1). On LR analysis, higher pre-treatment FiO2 and inability to eliminate shunt was associated with higher odds of composite outcome (Table 2). A stepwise increase in mortality was observed with worsening PDA status post-treatment (Table 3). A reverse association existed with NEC and BPD among participants, potentially owing to survival bias.
Conclusion(s): The rates of shunt elimination with primary treatment are extremely poor with current therapeutic regimes in ELGANs. When occurs, early shunt elimination with medical treatment may be associated with lower mortality but higher morbidities among survivors.