Emergency Medicine
Session: Emergency Medicine 7: Emergency Medical Services
222 - Acute Respiratory Failure in Children after Interfacility Emergency Department Transfer
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 222
Publication Number: 222.2071
Publication Number: 222.2071
- KJ
Kaileen Jafari, MD (she/her/hers)
Assistant Professor
University of Washington School of Medicine
Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Emergency department(ED) interfacility transfer of acutely ill pediatric patients has inherent risks, including clinical deterioration due to unrecognized illness severity and progression of disease. Among the most worrisome of these risks is the development of acute respiratory failure, as such patients may need critical interventions and pediatric intensive care. However, the predictors of acute respiratory decompensation in children after ED interfaculty transfer has not been fully characterized.
Objective: To determine the patient, visit, and hospital characteristics associated with acute respiratory failure in children after ED interfaculty transfer in 4 U.S. states.
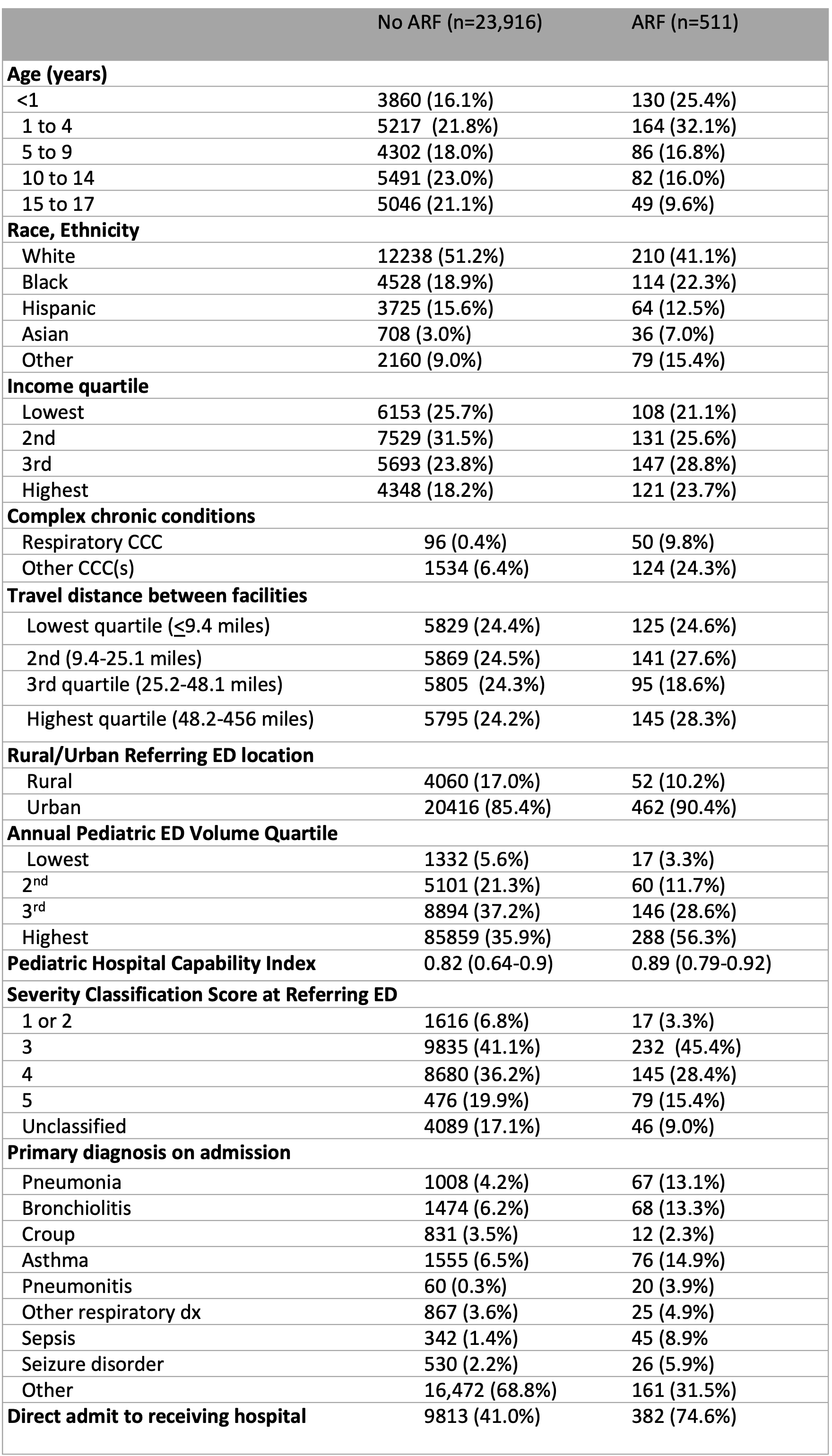
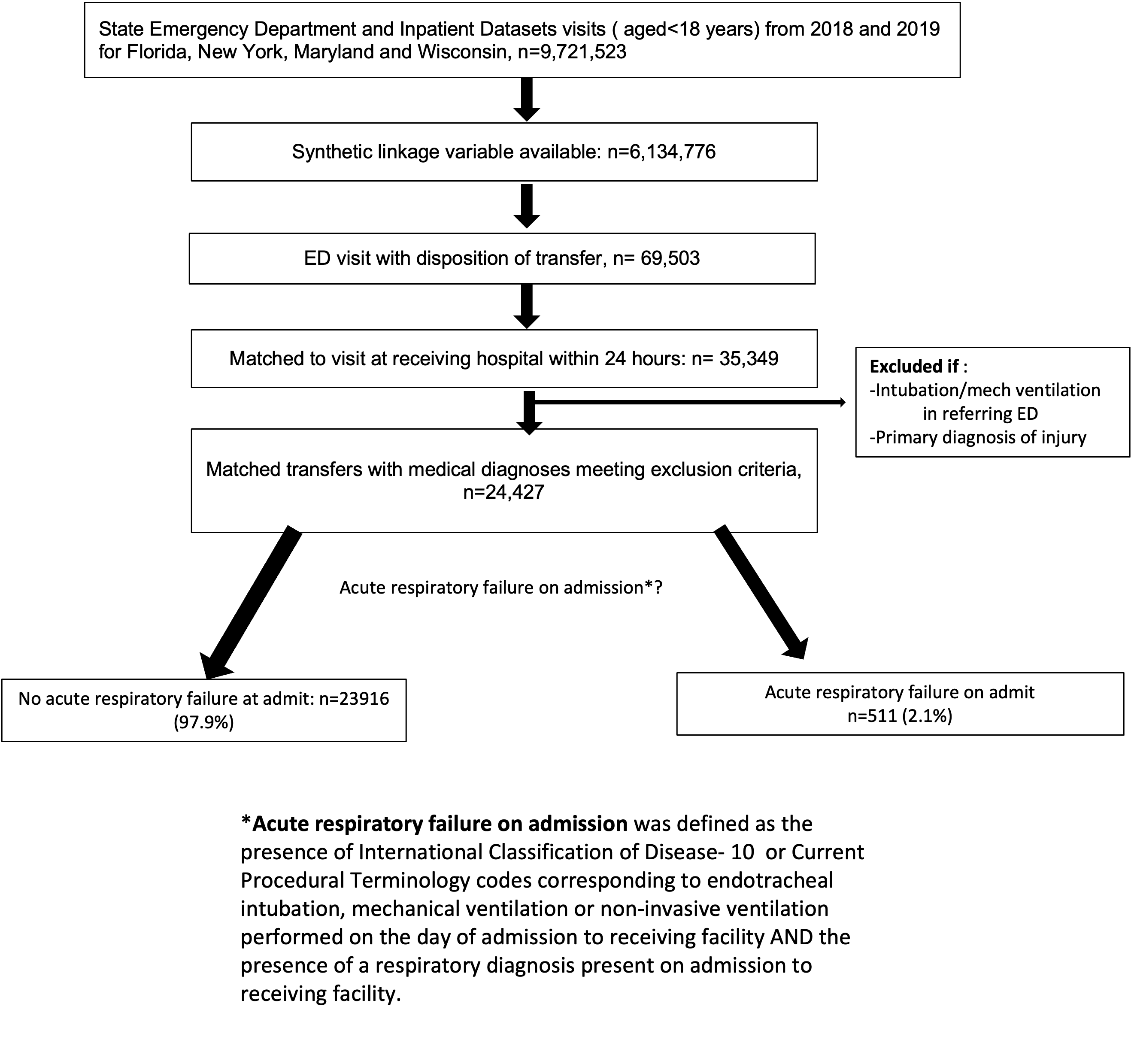
Design/Methods: Cross-sectional analysis of Health Care Utilization Project State ED and Inpatient Datasets from 2018, 2019. ED transfers aged < 18 years that were matched to an encounter at a receiving hospital within 24 hours were included. Figure 1 details the methodology of sample selection and identification of ARF visits. Descriptive statistics were used to characterize patient, hospital, and visit characteristics of pediatric transfers with and without ARF. Logistic regression was used to determine variables associated with ARF.
Results: Of 24,427 matched transfers, 2.1%(n= 511) had ARF on admission to the receiving hospital. The transfers with ARF were predominantly aged < 5 years( n=294, 57.5%), from the highest two quartiles of pediatric ED volume(n=433, 84.9%) and had a primary diagnosis of a respiratory illness(n=243, 47.5%), sepsis (n=45, 8.9%), or seizure(n=43, 7.2%)(Tables 1). In the logistic regression model, Asian race (OR 1.9 95%CI 1.2-2.9), chronic respiratory comorbidities(OR 7.9 95%CI 4.9-12.8) and those with diagnoses of sepsis (OR 3.94 95% CI 2.49-6.23) and pneumonitis(OR 6.26 95%CI 3.23-12.1) had the highest odds of ARF. Longer travel time between hospitals (OR 1.8, 95% CI 1.3-2.5) , higher pediatric capability of the referring ED (OR 1.7 95%CII 1.1-2.6) , and direct admissions (OR 3.6 95% CI 2.8-4.4) were also associated with higher odds of ARF after ED transfer.
Conclusion(s): Acute respiratory failure after ED transfer was infrequent overall( 2.1%), but those who were younger, of Asian race, admitted for pneumonitis or sepsis , had a history of chronic respiratory conditions, and had longer travel times between facilities were at highest risk of ARF after ED transfer. These findings may help guide pre-transfer ED care and transport decisions for children at risk of respiratory deterioration during transport.
.png)