Emergency Medicine
Session: Emergency Medicine 3: Serious Bacterial Infections
98 - Blood enterovirus and parechovirus polymerase chain reaction testing in young febrile infants
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 98
Publication Number: 98.1333
Publication Number: 98.1333
.jpg)
José Antonio Alonso Cadenas (he/him/his)
Pediatric Emergency Physician
Pediatric Emergency Department. Niño Jesús University Hospital
Madrid, Madrid, Spain
Presenting Author(s)
Background: The rate of invasive bacterial infection (IBI) in known cases of enterovirus is lower than for febrile infants without these infections. Polymerase chain reaction (PCR) tests have led to the rapid identification of enterovirus, although there is still little evidence to consider positive enterovirus infants as in low risk for IBI. In fact, management strategies such as the PECARN rule and the Step-by-step approach have not included this PCR test in the emergency department (ED) evaluation of these infants.
Objective: To analyze the prevalence of IBI (bacterial pathogen in blood or cerebrospinal fluid) in infants ≤90 days of age with fever without a source (FWS) and normal urine dipstick by the result of blood enterovirus and parechovirus PCR testing (ev-PCR).
Design/Methods: Observational multicenter prospective study including infants ≤90 days of age with FWS attended at 5 Spanish pediatric EDs between October 2020 and September 2023. We included all febrile (≥38ºC) infants with a normal urine dipstick (no leukocyturia or nitrituria) and a blood ev-PCR and blood culture (BC) obtained. We excluded those infants lacking relevant test results (BC, ev-PCR), those who received antibiotic treatment in the previous 48 hours and those whose caregivers refused to participate. All infants were followed up by telephone or revision of unscheduled visits reports for 4 weeks after the initial ED visit.
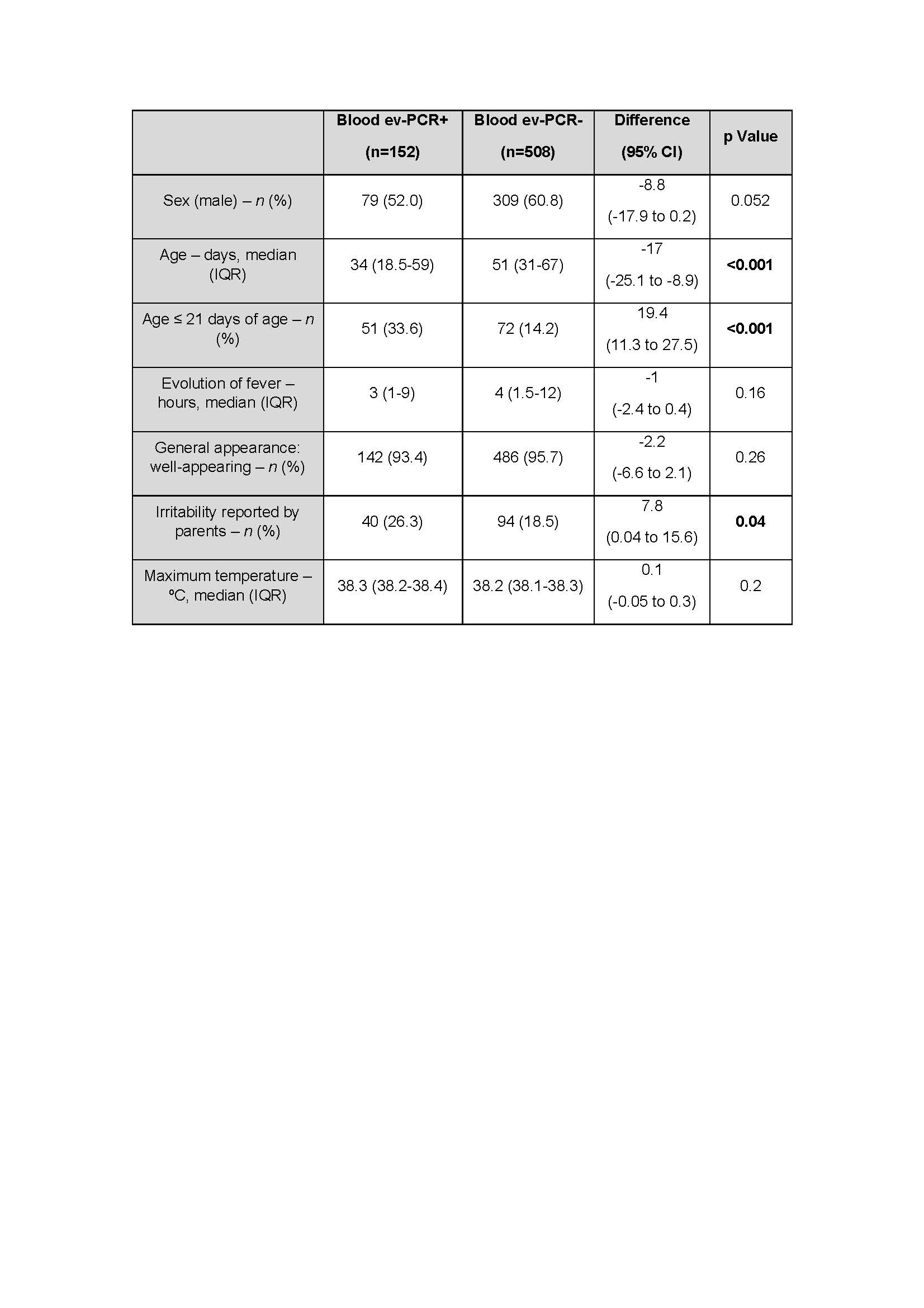
Results: Among 919 infants ≤90 days of age with FWS and normal urine dipstick attended, 660 (71.8%) were included in the analysis (table 1). Of them, 21 (3.2%) were diagnosed with an IBI, all of them bacteremia. The most common isolated microorganisms were S. agalactiae 8, S. aureus 4, and E. coli 3. Three of them associated meningitis (S. agalactiae 2, S. gallolyticus 1). The blood ev-PCR was positive in 152 (23.0%) infants. Only one of the patients with a positive blood ev-PCR test was diagnosed with an IBI [0.7% (95% CI 0.02% to 3.6%) vs 3.9% (95% CI 2.4% to 6.0%) of those with a negative blood ev-PCR test; (p=0.04)]. The three patients diagnosed with a bacterial meningitis had a negative blood ev-PCR result.
The infant with a positive ev-PCR and a concomitant IBI was a well-appearing 54-day-old boy with normal blood tests and a bacteremia by S. pyogenes.
Conclusion(s): Young febrile infants with a positive blood ev-PCR have a low risk of IBI, despite being younger and presenting more frequently with irritability. Including the blood ev-PCR test in the clinical decision-making may help to avoid unnecessary hospitalization and antibiotic treatment.