Neonatology
Session: Neonatal/Infant Resuscitation 1
267 - OpTuPos: Optimal Nasotracheal Tube Positioning in Term and Preterm Neonates
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 267
Publication Number: 267.3047
Publication Number: 267.3047

Susanne Tippmann, MD (she/her/hers)
neonatologist
University medical center, Mainz
Mainz, Rheinland-Pfalz, Germany
Presenting Author(s)
Background: Intubation of preterm and term neonates is a challenging procedure, and optimal tube insertion depth is important to avoid adverse events and provide safe ventilation.
Objective: There are several tables and charts recommending nasotracheal tube insertion depths, but there is limited data to support these recommendations. The aim of this study was to develop reliable and user-friendly recommendations for optimal nasotracheal tube insertion depth.
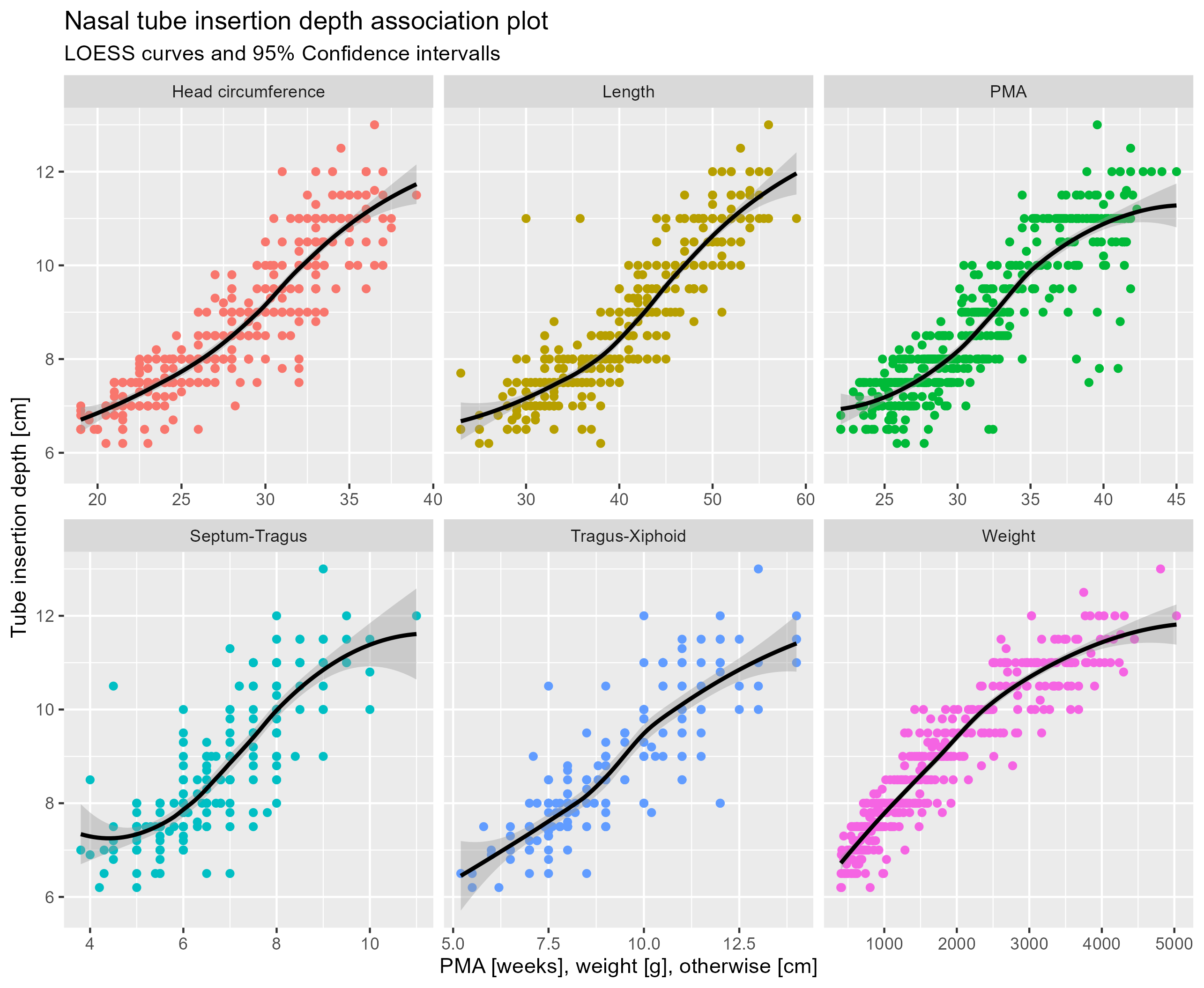
Design/Methods: This prospective, observational study analyzed all consecutive data from nasotracheal intubations performed between 2017 and 2023 in a single-center, tertiary care neonatal unit. Final and correct tube insertion depths were documented in a self-administered sheet, as were infant characteristics at the time of intubation. We defined correct tube position on the chest radiograph as the tip of the tube in the segment between the medial clavicle and 1 cm cranial to the tracheal carina in a neutral position. Based on the LOESS curves analysis and 95% confidence intervals, a linear regression model (R version 4.2.3) was developed to identify the optimal linear relationship between tube insertion depth and postmenstrual age and several anthropometric parameters.
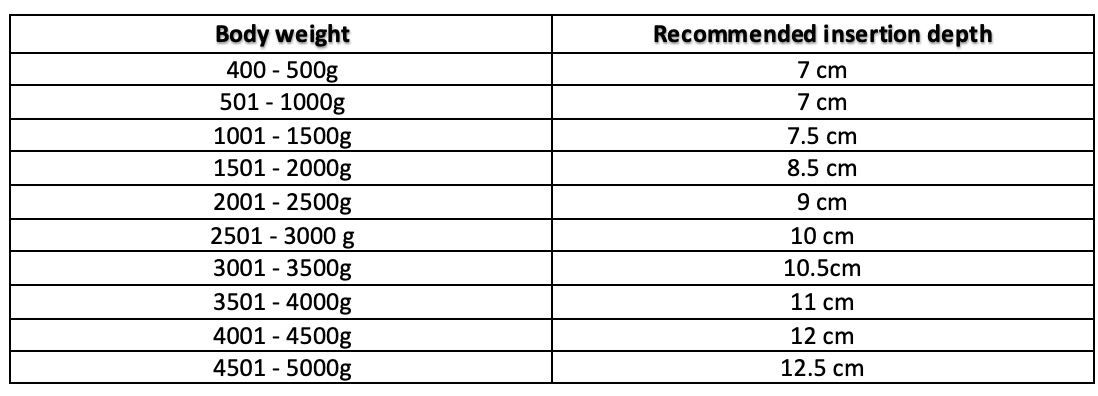
Results: A total of 496 nasotracheal intubations were evaluated. Correct tube insertion depth was correlated with postmenstrual age (PMA) (n = 496), current body weight (n = 495), body length (n = 463), head circumference (n = 461), nasal septum to tragus distance (n = 281), and tragus to xiphoid distance (n = 219) (Figure 1). Current body weight showed the best model performance (adjusted R2 0.883, root mean square error 0.516). Based on this model, a simplified table of recommendations for nasotracheal tube insertion depth was developed for infants weighing between 400 and 5000 g (Table 1). The most accurate recommendations are provided by a newly developed digital application that displays the results of a calculation model combining all available data based on regression analyses and power calculations.
Conclusion(s): We provide reliable and easy-to-use recommendations for nasotracheal insertion depth using calculation models based on either single or a combination of available infant characteristics. Prospective use may allow for verification of accuracy and ongoing refinement through new data entry.