Neonatology
Session: Neonatal/Infant Resuscitation 2
283 - A Comparison of Neonatal Outcomes of Term Neonates with Meconium-Stained Amniotic Fluid Before and After Routine Endotracheal Suctioning Strategy at Birth
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 283
Publication Number: 283.2743
Publication Number: 283.2743
- SC
Sanjay Chawla, MD (he/him/his)
Professor of Pediatrics
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Recent NRP guidelines no longer recommend routine immediate endotracheal (ET) suctioning for infants born through meconium-stained amniotic fluid (MSAF) . There are no RCTs in high-income countries to assess outcomes with this change. It is possible that some neonates that were classified as non-vigorous previously could be labeled as vigorous with immediate stimulation after birth per current guidelines by medical practitioners, making it important to compare outcomes of both non-vigorous and vigorous neonates with MSAF
Objective: To compare the incidence of meconium aspiration syndrome (MAS), the incidence of NICU admission, and other neonatal morbidities among all and non-vigorous neonates with MSAF born before and after this practice change
Design/Methods: A multicenter retrospective chart review of infants (GA≥ 36 wks) born between November 2012 and November 2018 with presence of MSAF. Patients were classified into 2 categories: Era 1- November 2012- October 2015, when routine ET suctioning was performed, and Era 2- January 2017- November 2018, when routine ET suctioning was not performed. MAS was defined as the presence of respiratory distress and receipt of respiratory support in the presence of MSAF
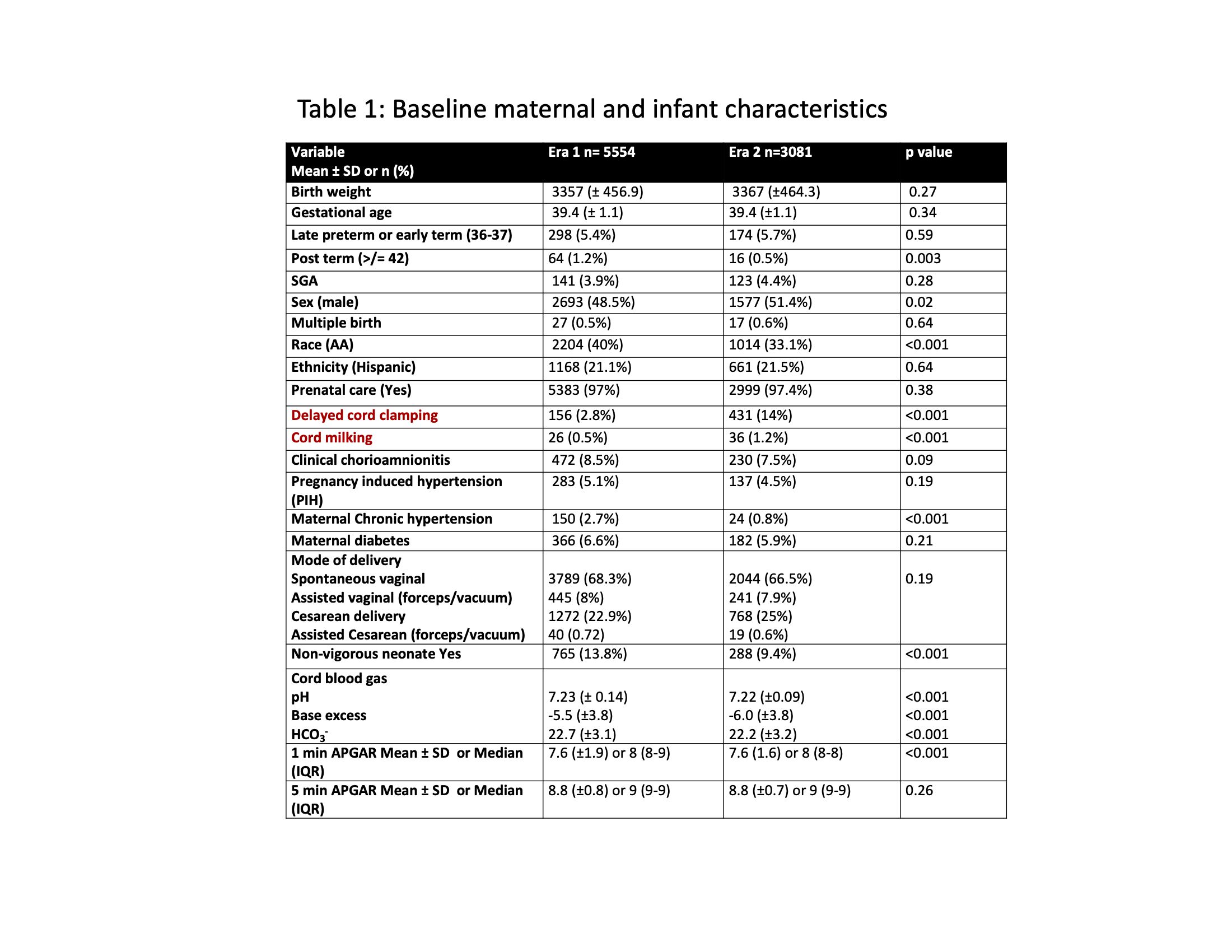
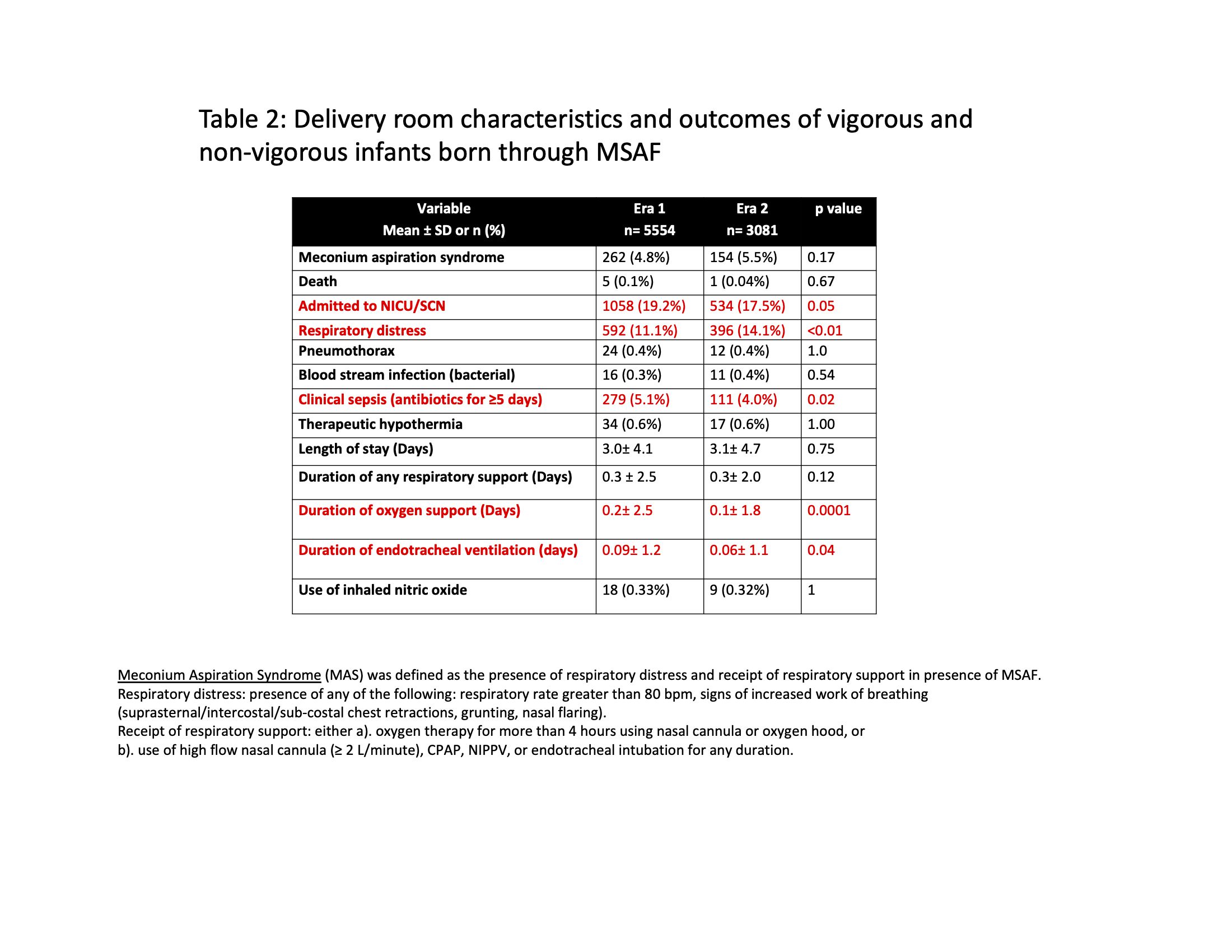
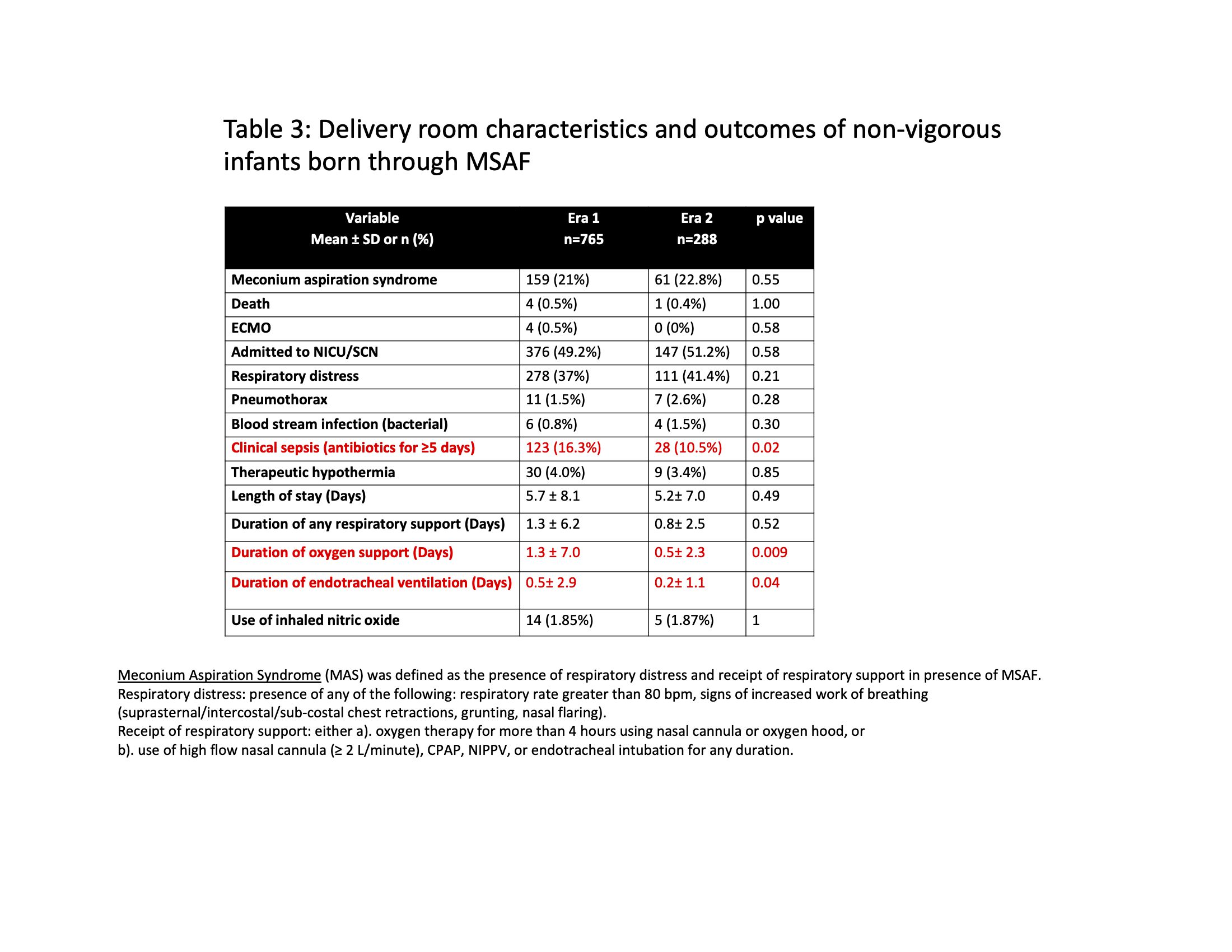
Results: Study cohort included 5554 neonates in Era 1 and 3081 neonates in Era 2. A higher proportion of infants were categorized as non-vigorous in era 1: 765 (13.8%) vs. 288 (9.4%) in era 2. (Table 1). Among all neonates, as well as among non-vigorous neonates with MSAF there was no change in MAS. Among all neonates with MSAF, there was a significant reduction in the rate of NICU admission, clinical sepsis, duration of oxygen and invasive ventilation, but an increase in rate of clinical respiratory distress in era 2 (Table 2). Among non-vigorous neonates, there was a significant reduction in the rate of clinical sepsis, duration of oxygen, and invasive ventilation in era 2 (Table 3)
Conclusion(s): In this large observational study, we found discontinuation of ET suctioning in non-vigorous meconium-stained infants did not result in an increased risk for MAS. Among all infants born through MSAF, discontinuation of ET suctioning was associated with a reduced rate of NICU admission, clinical sepsis, duration of oxygen and invasive ventilation, but with an increased risk of respiratory distress. Among non-vigorous neonates, there was a reduced rate of clinical sepsis, duration of oxygen and invasive ventilation. We believe these conflicting results support the need for an appropriately powered multicenter RCT in high-income countries evaluating ET suctioning in non-vigorous infants born through MSAF