Neonatology
Session: Neonatal Cardiology and Pulmonary Hypertension 2: BPD and prematurity
102 - Hemodynamic phenotypes in congenital diaphragmatic hernia and their association with morbidity and mortality
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 102
Publication Number: 102.2279
Publication Number: 102.2279

Daniel Ibarra-Rios, MD (he/him/his)
Neonatology-POCUS
Instituto Nacional de Perinatologia
Mexico City, Distrito Federal, Mexico
Presenting Author(s)
Background: Congenital diaphragmatic hernia (CDH) is a serious pathology with high morbidity and mortality. Its severity is related to the degree of pulmonary hypoplasia; Recently, the importance of different hemodynamic phenotypes (HP) has been described.
Objective: To describe and analyze the HP found in patients with CDH, their baseline, pre- and post-surgical echocardiographic follow-up, and their association with management and morbidity and mortality.
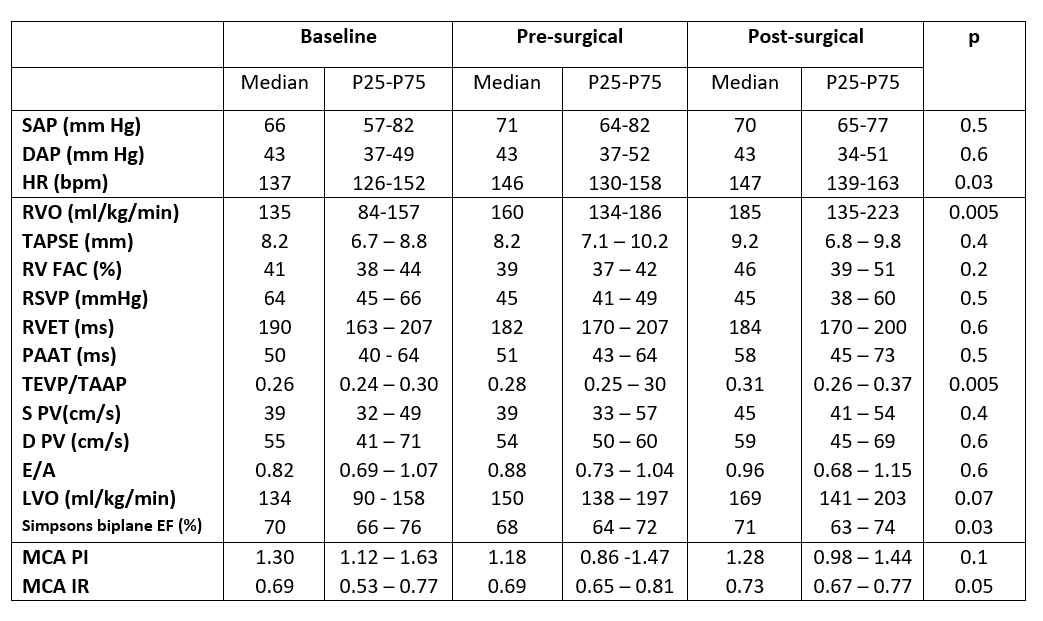
Design/Methods: All patients with CDH assessed by targeted neonatal echocardiography from January 2017 to April 2022 were included. The differences between survivors and non-survivors were compared with U Man Whitney's test; baseline, pre and post surgical echocardiographic parameters with Wilcoxon test and survival curves with Kaplan Meyer.
Results: A total of 28 neonates were included, with 24 survivors (86%). HP were classified in 3 groups: HP1. Mild pulmonary hypertension (PH) without ventricular dysfunction (n=9), HP2 (Pre-capillary PH phenotype). Moderate to severe PH/right ventricular dysfunction (n=8), HP3 (Post-capillary PH phenotype). Moderate to severe PH with left ventricular dysfunction/biventricular dysfunction (n=11). Patients were treated according to the physiology found [Figure 1]. Two died after surgery and two without surgery. Factors associated with mortality were higher pCO2, lower left ventricular output (LVO) and higher pulmonary vascular resistance (PVR) [Table 1]. Survival curves were calculated, finding a non-significant trend towards higher mortality in HP2 (one death) and HP3 (three deaths). At follow-up, a gradual increase in biventricular output, a decrease in PVR, and compensatory cerebral vasodilation (p ˂ 0.05) were observed [Table 2].
Conclusion(s): Hemodynamic phenotypes were related to patient mortality, who presented in those with greater pulmonary hypoplasia and suboptimal ventricular performance. Post-capillary PH phenotype had higher mortality. Echocardiographic follow-up showed an increase in biventricular performance, a decrease in PVR that allows the repair of the defect, and an adaptation of cerebral perfusion.
.jpg)
.jpg)