Neonatology
Session: Neonatal General 9: Outcomes, Genetics. Ethics
390 - Comparison of Outcomes of Infants Admitted to the Neonatal Intensive Care Unit Who Needed Pharmacologic versus Non-Pharmacologic Intervention Prior to Magnetic Resonance Imaging
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 390
Publication Number: 390.2965
Publication Number: 390.2965
- HQ
Hashir Qamar, DO (he/him/his)
Resident Physician
Los Angeles General Medical Center
Los Angeles, California, United States
Presenting Author(s)
Background: Magnetic Resonance Imaging (MRI) is widely utilized in the Neonatal Intensive Care Unit (NICU). To optimize imaging, non-pharmacologic intervention such as immobilization board, feeding prior to procedure, non-nutritive sucking, and facilitated tucking are used. Some neonates may require pharmacologic intervention in the form of opioids or benzodiazepines. The use of sedation in neonates has potential risks and adverse effects, including progression to deep sedation or obtundation, death, increased respiratory support, and adverse neurodevelopmental outcomes.
Objective: To assess the rate of infants requiring pharmacologic intervention to complete an MRI procedure and determine its adverse effects.
Design/Methods: Retrospective cohort study of all neonates admitted to the NICU who underwent brain MRI from January 2021 to June 2023. Neonatal demographics, MRI indication, MRI duration, respiratory support before and after imaging, feeding intolerance, and length of stay were obtained from electronic medical records and Neonatal Information System Database. Infants were divided into 2 groups based on whether they received pharmacologic intervention with MRI. Chi Square and Wilcoxon rank sum was used for categorical and continuous variables. McNemar test was used to determine the difference in respiratory support before and after MRI.
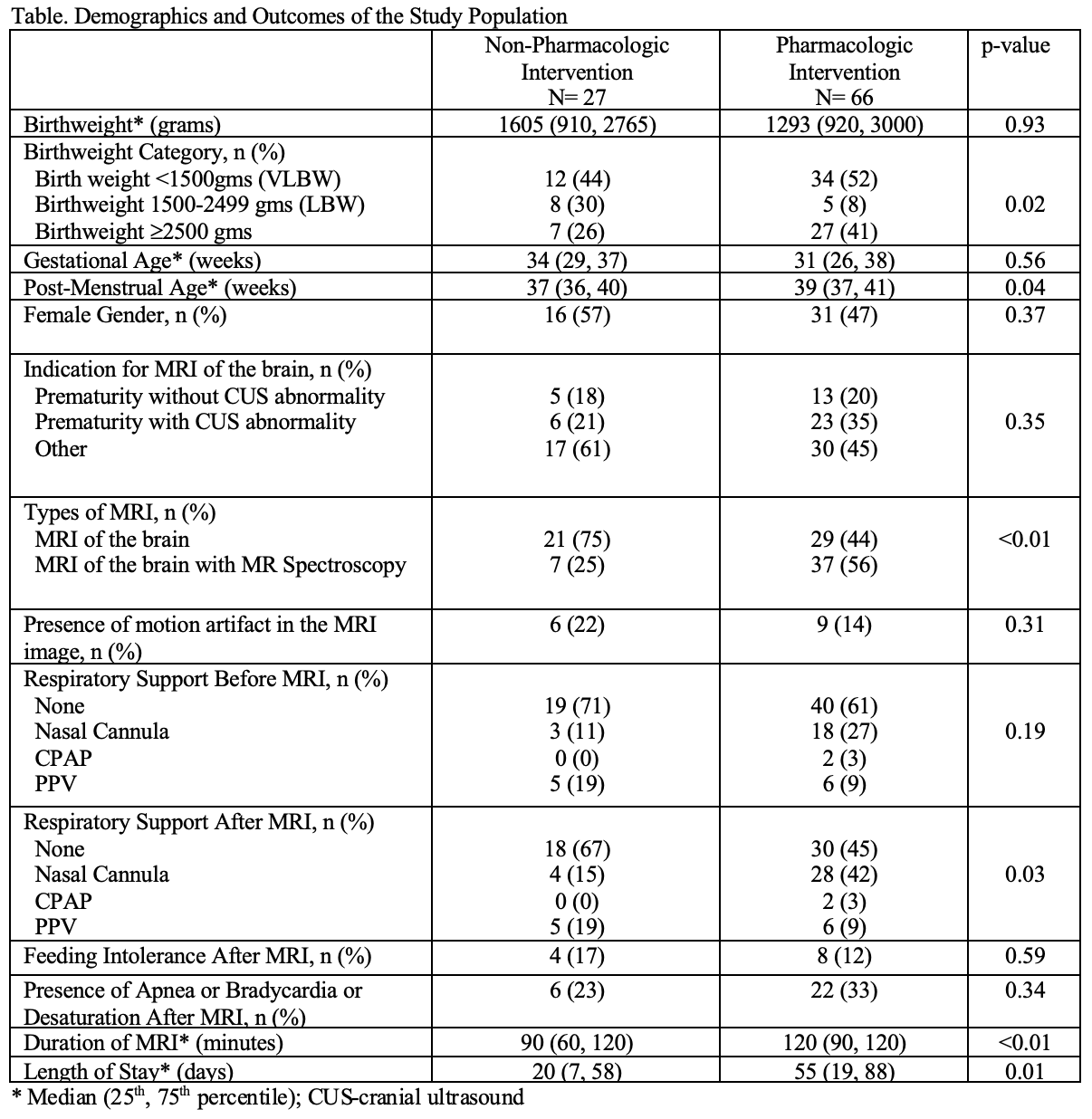
Results: 94 neonates underwent MRI during the study period. Majority of the neonates 66/94 (70%) received pharmacologic intervention in the form of midazolam 63/66 (95%), fentanyl 2/66 (3%) and morphine 1/66 (2%) to complete the MRI. There was no significant difference in gender, gestational age, birthweight or MRI indication between groups. Majority of neonates who required pharmacologic intervention were very low birth weight (VLBW) infants, had significantly higher post menstrual age, higher rate of additional MR spectroscopy procedure in addition to MRI, longer stay in the MRI suite and were more likely to need escalation of respiratory support after MRI (Difference 0.15, 95% CI: 0.04, 0.26 p value < 0.01) There was no significant difference in feeding tolerance or occurrence of apnea, bradycardia, and oxygen desaturations after MRI between the two groups. (Table)
Conclusion(s): Our preliminary data showed that neonates requiring pharmacologic intervention to complete the MRI were more likely to be VLBW, needed additional imaging and stayed in the MRI suite longer. Pharmacologic intervention may have led to escalation of respiratory support. We need to limit the duration of MRI, avoid additional imaging and maximize non pharmacologic measures to limit the use of sedation.